You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The message delivered to dental patients was fairly consistent for more than a half century: proper homecare (consisting of regular brushing and flossing) plus regular maintenance visits (focused on removing calculus and plaque that could be seen and felt) were the key to oral health. Dentists were seen to be in the tooth-cleaning or even tooth-saving business. However, in recent years, it has become apparent that the stakes are far higher. With recognition of the oral–systemic connection and a better understanding of the etiology of periodontal disease,1 it now appears that dentists should actually be in the business of reducing inflammation because its consequences go far beyond the mouth, as suggested in a 2004 Time Magazine cover story, which called inflammation “The Secret Killer.”2
A NEW UNDERSTANDING OF PERIODONTAL DISEASE
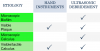
It was previously believed that periodontal disease was simply caused by bacteria that calcify, and that scraping off everything that could be seen or felt would lead to good health (Figure 1).1 But, as it turns out, that is not necessarily the case.
The etiology of disease—biofilm—cannot always be detected and removed as previously thought.2 This changes everything in terms of which patients should be seen and treated, which sites are treated, and defining the endpoint of treatment.
It is also now clear that although bacteria initiates the disease, there is a very complex host response to that initiating bacteria that goes beyond its oral impact; as suggested by recent findings, the ramifications are systemic as well as oral.3 Treatment success, therefore, is maximized by addressing both the bacterial burden and the host response.
THE ORAL–SYSTEMIC LINK EXPLAINED
Biofilm
Biofilm describes what bacteria do anywhere when they are in an aqueous environment—whether it is in the mouth, in the body, or in nature. By design, bacteria form biofilm communities. They secrete proteoglycans and other substances, and the general feeling is that the bacteria do this as a protective mechanism.4 They form primitive colonies, three-dimensional communities that give them protection and make them less susceptible to antimicrobial agents. This is the reason why periodontal disease cannot be eliminated by systemic antibiotic therapy. Also, because this biofilm is not deeply embedded into the cementum—existing only in the outer 40 microns—the aggressive cementum removal previously taught was likely not helpful.5
Inflammatory Response to Bacteria
It is now known at the ultra-structural level that bacteria in the form of biofilm accumulates between the soft tissue and the tooth, and if that bacteria is left undisturbed long enough—either because it is not adequately removed on a regular basis or the hygienist is not adequately removing the etiology—that initiating bacteria chemotactically attract inflammatory cells, most notably white blood cells into the area, which sets up a low-grade chronic inflammatory response.6
The white blood cells then offload a variety of inflammatory mediators meant to neutralize the bacteria. While those mediators are quite helpful in neutralizing insults such as bacterial infections, a downside is that they actually cause collagen to dissolve. Given that the root surface, periodontal ligament fiber, and connective tissue are mostly collagen, in losing the connective tissue and the collagen support, integrity in the lining epithelia is lost as well. When collagen is destroyed, and integrity is lost in the lining epithelium, there is typically bleeding on probing in the periodontal pocket.7
Platelet Aggregation-Associated Protein
Another issue is that specific bacteria that can be part of the normal oral flora have a platelet aggregation-associated protein, so when periodontal disease is allowed to persist in patients who have these bacteria as part of their normal flora, those bacteria spill into the bloodstream and cause platelets to come together. That is one of the mechanisms by which periodontal disease is linked with cardiovascular disease.8
Tissue Necrosis Factor
The inflammatory mediators that are released orally similarly play a role in systemic involvement. TNF—tissue necrosis factor alpha—for instance, has long been known to suppress insulin activity both directly and indirectly.9 Therefore, if a patient with diabetes—who already is at increased risk for developing periodontal disease—does develop it and and is not maximally treated, those oral periodontal cells produce a significant amount of tissue necrosis factor-alpha, which then can spill into the bloodstream and adversely affect insulin. Patients with diabetes who have periodontal involvement then have a more difficult time controlling their blood sugar.10
The Inflammation-Dependent Relationship
The mechanism by which oral and systemic health are linked is that the relationship is inflammation-dependent. Inflammation opens the portal of entry that allows the bacteria and its byproducts to travel through the ulcerated epithelium into the bloodstream and enter this systemic circulation. By eliminating inflammation, it is possible to reestablish the integrity of a epithelium lining, close the portal of entry, and reduce or eliminate the risk for these serious chronic diseases when periodontal disease is present.11
SUPPRESSING INFLAMMATION
Given the findings linking inflammation from periodontal disease to everything from low birth-weight babies and cancers, as well as cardiovascular disease and diabetes, suppressing inflammation takes on added significance not only from an oral health-oriented diagnostic and treatment outcome standpoint, but also from a total health standpoint.12 Clearly, the stakes are higher in this new world of periodontal inflammation.
Where Pocket Depths Come In
The main goal of periodontal therapy has always been to reduce pocket depths. Now, in keeping with the new emphasis on reducing inflammation as both a diagnostic and therapeutic outcome, inflammation—as evidenced by persistent bleeding on probing—is used to determine when to treat, but it is pocket depths that are used to determine how to treat, as shown in the algorithm detailed in Figure 2.13
Questions to Ask
Question number 1 is: “Is there inflammation present at the site?” If the answer is yes, it is the probing depth of that site that helps to determine the approach to treatment. But if the answer is no, the clinician needs to determine the likelihood that it can remain inflammation-free based on whether it can be properly maintained and/or debrided, and decide whether or not treatment is indicated.
Identifying Inflammation
In practical terms, it makes sense to focus on the problem areas—ie, where there is clear presence of inflammation—although it is not always readily apparent. For example, inflammation can be masked in tobacco users because the nicotine and its metabolite cotinine actually have a vasoconstrictive effect.14 Further, some amount of bleeding is to be expected, and not even all persistent bleeding leads to attachment loss.
While going quadrant by quadrant and site by site with their probe, clinicians should be looking for evidence of apparent inflammation and/or bleeding—whatever the probing depth—and measuring the probing depth at those areas of inflammation to prepare a “battle plan” for sites that require maximum effort. The author believes that the best way to identify worrisome persistent bleeding is to chart it.
Patient-Specific Issues
Clinicians also need to keep in mind the questions concerning whether the patient can regularly maintain or debride the area. Further they should be aware of that maximizing the chance for treatment success is particularly critical in patients with risk factors for or who already battle systemic diseases.
AN APPROACH TO TREATMENT
Gathering Information
The most important information for the clinician is to know exactly where the problem sites are by gathering this information: (1) the location of each site where inflammation is present; (2) how long the inflammation has persisted; (3) the probing depth of the sites where inflammation is present; (4) the risk profile of the patient; (5) the patient’s treatment history.
Understanding the Role of Home Care
It is the author’s belief that brushing and flossing have no effect on existing subgingival inflammation. They are not a treatment for periodontal disease but, rather, a strategy to prevent relapse of disease.
Subgingival Debridement
Questions About Traditional Approaches
Given the current understanding of how bacteria forms and why previous approaches—removing calculus and plaque that can be seen and felt and aggressive removal of cementum—have proven inadequate, it is clear that different approaches are needed.
Because it is now understood that proteins in the cementum may actually stimulate a better level of attachment, striving to achieve a hardcore, glass-smooth surface is no longer recommended.15
But knowing that the etiology has a microscopic component, it is prudent to reexamine whether traditional hand instrumentation actually maximizes the removal of disease etiology in all of its forms.
Ultrasonic Debridement
The author was among the contributors to the first-ever comprehensive textbook on ultrasonic periodontal debridement, which was published last year.16 While a review of the literature indicated that debridement with traditional hand instrumentation and ultrasonic technology yield identical outcomes, these results were achieved under ideal laboratory circumstances, which may not reflect clinical practice performance.17
There is no question that, in terms of positioning and level of force directed at the outer 40 microns, ultrasonic debridement is easier than hand instrumentation to use properly and, therefore, much more predictable.
Ultrasonic debridement has other advantages as well, including cavitation. Inserts of different shapes enable the practitioner to maximize intimate contact between the insert and the root surface (Figure 3 and Figure 4). The vibration of the tip mechanically interrupts the etiology in all of its forms and also exerts the cavitational effect, the energy that is imparted through the frequency of movement, and the millions of tiny bubbles that form and then implode the released energy. While there is some debate about whether that energy kills bacteria, there is complete consensus that cavitation has the ability to disrupt biofilm beyond the insert tip.18
Therefore, with ultrasonic instrumentation, it is possible to widen the area of debridement, making it more likely to maximize the chance of removing the etiology, including microscopic as well as visible and tactile calculus and plaque (Figure 5).
So while sonic and hand instrumentation may have equal ability to remove plaque and calculus that are visibly or tactilely evident and to interrupt microscopic biofilm, ultrasonic debridement has significant debridement advantages, not only because it is easier to use properly, but because it also offers the cavitational effect.
Endpoint/Goal of Therapy
The goal of therapy can be considered to be converting a bleeding to a nonbleeding site, which research suggests results in histologic health.19 This absence of bleeding can be used toconfirm that the integrity in the lining epithelium is restored—ie, that, as a result of therapy, that portal of entry for bacteria and the mediators of inflammation has been closed.
However, it is essential to look forward and acknowledge that the achievement of that endpoint—ie, the lack of chronic inflammation or stable and maintainable probing depths—requires ongoing vigilance and preventive treatment. Clinicians must do whatever is necessary to help patients achieve and maintain a preferred level of oral health.
Conclusion/Summary
The takeaway of this discussion is that clinicians can no longer take a now-you-see-it—or feel it—approach to periodontal debridement therapy. They should assume that microscopic biofilm covers the entire surface at a site where persistent inflammation is present (Figure 6). At those problem sites, removal of just the visible calculus may not be sufficient. And now, with the advent of the understanding that persistent inflammation has ramifications outside of the mouth, it is important to not only remove the visible and tactile calculus but also the remaining root surface using a method that enables the hygienist to interrupt any potential microscopic etiology and to do it without excessive cementum removal in order to maximize the chance for resolution.
Therefore, dentists need to know (1) where there is inflammation; (2) whether that inflammation has been persistent; and (3) the probing depth of those sites of inflammation.
Based on that information, they should use a debridement method that allows them to maximize the chance of removing the microscopic—as well as the visible/tactile—etiology without any cementum removal. In this regard, ultrasonic instrumentation offers tremendous benefits.
Inflammation leads to many chronic diseases of aging. Maximizing the chance for the elimination of subgingival inflammation over the lifespan of a patient is essential not only to maintain their oral health but also to help them maintain their overall health.
About the Author
Dr. Donley is a private practitioner from Bowling Green, Kentucky.
References
1. White DJ. Dental calculus: recent insights into occurrence, formation, prevention, removal and oral health effects of supragingival and subgingival deposits. Eur J Oral Sci. 1997;105(5 Pt 2):508-522.
2. Thomas JG, Nakaishi LA. Managing the complexity of a dynamic biofilm. J Am Dent Assoc. 2006;137 Suppl:10S-15S.
3. Genco RJ. Host responses in periodontal diseases: current concepts. J Periodontol. 1992;63(4 Suppl):338-355.
4. Schaudinn C, Gorur A, Keller D, et al. Periodontitis: an archetypical biofilm disease. J Am Dent Assoc. 2009;140(8):978-986.
5. Zaura-Arite E, van Marle J, ten Cate JM. Conofocal microscopy study of undisturbed and chlorhexidine-treated dental biofilm. J Dent Res. 2001;80(5):1436-1440.
6. Campbell L, Millhouse E, Malcolm J, Culshaw S. T cells, teeth and tissue destruction - what do T cells do in periodontal disease? Mol Oral Microbiol. 2015 Oct 27. doi: 10.1111/omi.12144. [Epub ahead of print].
7. Preshaw PM. Detection and diagnosis of periodontal conditions amenable to prevention. BMC Oral Health. 2015;15 Suppl 1:S5. doi: 10.1186/1472-6831-15-S1-S5. Epub 2015 Sep 15.
8. Perumal R, Rajendran M, Krishnamurthy M, et al. Modulation of P-selection and platelet aggregation in chronic periodontitis: A clinical study. J Indian Soc Periodontol. 2014;18(3):293-300.
9. Grauballe MB, Østergaard JA, Schou S, et al. Effects of TNF-α blocking on experimental periodontitis and type 2 diabetes in obese diabetic Zucker rats. J Clin Periodontol. 2015;42(9):807-816.
10. Simpson TC, Weldon JC, Worthington HV, et al. Treatment of periodontal disease for glycaemic control in people with diabetes mellitus. Cochrane Database Syst Rev. 2015 Nov 6;11:CD004714. doi: 10.1002/14651858.CD004714.pub3.
11. Ting CC, Fukuda M, Watanabe T. Morphological alterations of periodontal pocket epithelium following Nd:YAG laser irradiation. Photomed Laser Surg. 2014;32(12):649-657.
12. Chapple IL, Wilson NH. Manifesto for a paradigm shift: periodontal health for a better life. Br Dent J. 2014;216(4):159-162.
13. Hasturk H, Kantarci A, Van Dyke TE. Paradigm shift in the pharmacological management of periodontal diseases. Front Oral Biol. 2012;15:160-176.
14. Mavropoulos A, Aars H, Brodin P. Hyperaemic response to cigarette smoking in healthy gingiva. J Clin Periodontol. 2003;30(3):214-221.
15. Aimetti M. Nonsurgical periodontal treatment. Int J Esthet Dent. 2014;9(2):251-267.
16. George MD, Donley TG, Preshaw PM. Ultrasonic Periodontal Debridement: Theory and Technique. 2014; Wiley-Blackwell.
17. Drisko CL, Cochran DL, Blieden T, et al. Position paper: sonic and ultrasonic scalers in periodontics. Research, Science and Therapy Committee of the American Academy of Periodontology. J Periodontol. 2000;71(11):1792-1801.
18. Howlin RP, Fabbri S, Offin DG, et al. Removal of Dental Biofilms with an Ultrasonically Activated Water Stream. J Dent Res. 2015;94(9):1303-1309.
19. Lynch SE, Lavin PT, Genco RJ, et al. New composite endpoints to assess efficacy in periodontal therapy clinical trials. J Periodontol. 2006;77(8):1314-1322.