You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The topic of “post and core” is pertinent to both endodontics and general dentistry. For every clinician, there is a unique way in which to do successful post-and-core dentistry; the field is highly complex. However, within the complexity, it is possible to focus on developing expertise in a specific area that occurs at a high frequency in post-and-core dentistry: prefabricated posts. Clinicians are often curious about which post system is best, when in fact no post is the “best” post. The more conservative a clinician's access, the greater the likelihood of obtaining longevity from a root canal or restoration. This article explores methods for obtaining conservative access and ensuring clinical success.
Root-Canal Access
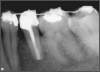
Ultimately, the aim in endodontics is to preserve the tooth as long as possible for the patient. A clinician may want to do a root canal but must face realistic concerns, such as not having enough tooth.1 Figure 1 shows a case where the clinician was able to access four canals through a zirconium crown, with limited access. Generally, it is preferable to err on the side of opening larger and cleaning out well. If the access is too small, three problems arise: (1) clinicians may not clean effectively; (2) there is a greater chance of separation because there is not enough of a straight path, and (3) canals may be missed. Conversely, if clinicians open too large, they can destroy the tooth. There is a happy medium where the result is fine-tuned and engineered perfectly. Although the perfect result is not always possible or ideal, clinicians continue to strive for it. The best approach is to find the canals and then open them up under a microscope to get enough access. This gives the clinician whatever shape is needed for conservative access.
Types of Posts
Many teeth need to be restored with posts, whether prefabricated metal posts, cast posts, or fiber posts. Fiber posts are currently the best option, but the most popular of the posts has been the prefabricated metal post.2 It is easier to use, cheaper, and provides more variability; clinicians can acquire many inexpensive and different sizes.3 Various options offer more flexibility, depending on the manner in which each case presents itself. The purpose of a post is to retain the core. Posts are used to retain composite, metal, or amalgam cores and help strengthen the connection between the coronal buildup material and the remaining tooth structure.
Principles of Post Placement
Certain principles must be accounted for to have a successful post and core.4 These principles can act as guidelines for the clinician: (1) quantity of tooth structure remaining, (2) quality of tooth structure remaining, (3) structures adjacent to the tooth, (4) occlusion and parafunctional habits, and (5) future restoration. Understanding the principles laid out in this article will enable clinicians to make the right decision based on the case at hand.
Quantity of Tooth Structure
When considering quantity, in general when more than half the tooth structure is missing, the clinician should consider placing a post. The issue is whether there is enough structure for retention of the crown. It depends on the ferrule, which can be defined as a 360-degree metal collar of the crown surrounding the parallel walls of the dentine extending coronal to the shoulder of the preparation.5 Sometimes the clinician has a situation where there is no ferrule, and other times the ferrule is almost ideal. The ideal is when there is no core, just the natural tooth functioning as the core, although there are exceptions.
In the ideal situation for restoring a tooth, there is 3 mm of the wall on one side and 2 mm on the other, which indicates at least a 2-mm ferrule.6 In this case, the clinician is going to have a higher chance of success. Restorations can occur in other situations, but the patient should be warned that failure is possible in certain scenarios.
Quality of Tooth Structure
When looking at the quality of the tooth structure, the clinician is looking for indications of non-ideal conditions, such as discoloration, cracks, an undercut, and concavities. The first premolar has a concavity, but sometimes there are concavities in molars, such as the distal of the lower molar or the palatal of the maxillary molar, eg, No. 3. These are teeth that should get posts. The clinician should aim to place the post in the straighter-path canal. On tooth No. 5, for example, it is usually the palatal. There are times when the straighter option could be another canal, such as the buccal, but generally the palatal is the best option.6
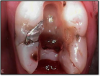
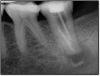
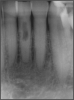
Figure 2 shows a situation where the clinician excavated the tooth of a patient with decay, and it pulped out. The buccal and lingual walls were intact; however, the walls were minimal, and there were still fragments of amalgam and cracks. If the clinician prepared this tooth after building it up, the clinician would lose all the good tooth structure that was left. This tooth would likely need a post.
Adjacent Structures
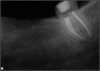
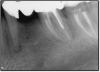
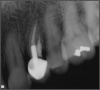
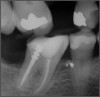
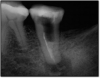
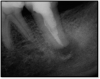
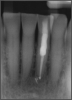
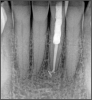
If a tooth stands alone, greater forces will be placed on it because it has no adjacent teeth to provide support. This situation will affect the decision-making process for placing a post. Figure 3 shows a tooth that was on an island and would be having three implants placed in front of it. The tooth would take a much greater beating than another tooth that had support proximally. Even though it had a good root canal, the clinician would need to account for whether the tooth would last until the implants integrated. Figure 4 shows a case that would quickly proceed to implants. The patient had a less-than-ideal bridge for over a decade, with decent endodontics and functionality. There was also an overhang on the premolar. The post was not ideal in this case because there was one distal canal and not all the gutta-percha was removed from it. An intimate fit should be the goal with the post and the walls. Whether using a threaded or non-threaded post, there should not be excess gutta-percha because it is not as solid as the tooth and will lead to greater movement. That movement on the tooth and bridge will create too much force and result in demise.
Figure 5 shows an interesting situation where a root tip was left from an old extraction. There was an area of necrotic tooth in the premolar that caused pain to the patient, who was also a heavy smoker. She had already experienced failure of three implants. When they failed, the clinicians tried to place just one implant slightly wider and thicker to resolve the issue, but that also had failed. Removing the bridge for an expensive treatment involving two implants and a new bridge was not an option. The clinicians needed to find a way to save the situation so her bite would remain optimal. They considered removing the bridge and replacing it with a long bridge from the molar to the canine adjacent to the premolar. They also considered a partial, because she was missing some teeth on the other side. After a lengthy discussion, they decided to do whatever they could to maintain her current bridge, planning to move to partials when the bridge failed.
Figure 6 shows the successful root canal that stopped the patient from being in pain, but she still had some discomfort. The images did not show anything significant; the case was completed at a time when cone-beam computed tomography (CBCT) was not routine. The clinicians had to trust what they saw, which was 6-mm probing that left a chance for a crack in the tooth. There was a buccal fracture of the mesial root. There was bone apical to it but nothing coronally, so they decided to resect the root. They cut it out, put some holes into the bone, and added demineralized freeze-dried bone. They also later put a collagen membrane over it and closed it.
This was not an ideal situation; the ideal would have been to take the bridge out and place implants, but that would not have been possible with a patient who had already experienced four implant failures. The implants that had failed were in the maxilla, so it was possible they would have been better in a different location, but it would also have been significantly more expensive.
The bridge that had lasted about 14 years managed to then last another 5.5 years before it cracked and failed. The question of whether the delay was worth the trouble was a personal choice only the clinician could make with the patient based on the unique circumstances. Because the post was not placed perfectly, it added stress that led to the mesial root cracking.
Occlusal Considerations
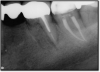
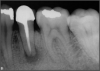
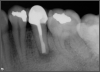
Occlusion is one of the most overlooked areas in endodontics; however, other than remaining structure, it is the most important factor.7 Patients who are heavy bruxers can cause the need for a root canal from the lateral forces. Patients who clench pose a different challenge with apical forces, yet the damage from both can be the same. Figure 7 shows a patient with bruxism. The patient had pain in response to hot and cold stimulus, and the clinicians needed a bitewing to determine which tooth was causing the pain. From the periapical (PA), it was clear that tooth No. 2 had a large problem, No. 3 had a crown, and No. 4 had a large restoration. Any of the three may have been the source of the problem.
With the bitewing shown in Figure 8, it became clear there was gross decay in tooth No. 3 that could not be seen on the PA, and there was a periodontal defect, a pulp stone, in No. 2. There was also a class V lesion revealing the bruxism, flat occlusion, multiple restorations in No. 30, a post in No. 31, and decay on No. 2 as well. The post in No. 31 was useless because when a post is placed, it must be the right length, width, and size. If the post is too short, there will be a greater fulcrum and the tooth will break. If it is too long, the clinician can break it by wedging it. If it is too short, it will not hurt the tooth, but it will not provide any valuable function. It is overall preferable to do posts in teeth having just single restorations rather than abutments for bridges because those teeth are already under greater force. If the technique is not performed correctly, iatrogenic issues may result.
Consideration of Future Restorations
Figure 9 shows a situation on tooth No. 12 that may have been presumed to be easily resolvable. However, the dentist experienced problems, including significant bleeding. It was due either to irreversible pulpitis or a perforation. Judging by the PA, something detrimental was occurring with the distal. A lesson that can be learned from this case is that a solution does not have to look pleasant for it to work. Functionally, the repair shown in Figure 10 was successful because the clinician was able to fix the whole wall with mineral trioxide aggregate (MTA) and was able to find the canal. The clinician also put in the post for the general dentist and closed it. Later, the general dentist took the post out and replaced it with a post that was larger and shorter than would be recommended. Interestingly, the result lasted 8.5 years, as shown in Figure 11.
The clinician took the path described because the patient initially came in with some sensitivity on the tooth, but the issue quickly progressed to the need for a root canal and the possibility of losing the tooth because her general dentist had inadvertently destroyed the wall. Unfortunately, the story does not have a happy ending: at 9.25 years, the repairs finally broke. Yet the case is important because it shows that a resolution for even a “terrible” case can last almost 10 years and be to some extent a success. When the right principles are maintained, there can still be a successful outcome. The reason this case in particular succeeded was because of a factor that was barely visible: above the perforation repair was 2 mm of ferrule and, therefore, coronal tooth structure. The perforation was not only below the gum but also the bone, which is generally a more ideal location for a perforation.
Figure 12 shows an example of a post that was too long. Although it was a pleasant-looking threaded post, there was about a millimeter of gutta-percha, where ideally 4 to 5 mm of gutta-percha would be used.8 This was also an iatrogenic problem where the referring dentist put a post directly into the furcation. This type of problem can be fixed by removal and repairing with MTA. However, because there was not much tooth structure, the tooth became far more compromised.
Figure 13 shows an example where there was likely a good root canal that was absorbed. The way to avoid this type of problem is that the person who does the root canal should do the post. This is not always possible, and some general dentists like to do the restorative work themselves, but the advantage of having the same person do both is that the person is familiar with the curve of that canal. That clinician also knows the thickness of the walls and what the canal will allow. In this case, it was done under a rubber dam, which was beneficial; often clinicians will see teeth that have good endodontics, but multiple years later, radiolucency will appear because when the post was placed, saliva seeped in.
The rules for placement of a post depend on good retention: the greater the length, the greater the retention.3 Also, two-thirds of the length of the root is ideal, but 4 to 5 mm of apical gutta-percha is essential because anything less than that will disrupt the seal.8 Figure 14 shows a case where a patient had a post, core, and crown. The threaded post was shorter than ideal because the tooth was longer. Not visible was the mental foramen underneath. The patient did not have the financial resources to have the case redone. However, when the post would be removed, the clinician would need to trephine or use an ultrasonic around it, making the access bigger than an ideal conservative access. Potentially, the crown would come off. The patient did not have finances for re-treating the tooth and could not have an apicoectomy because the mental foramen was directly under the tooth.
The options, therefore, were to extract it and put a bridge or an implant in later when funds were acquired, or, as was done in this case, perform an intentional replant. The clinician extracted the tooth, cut it, placed MTA, and then put it back under occlusion using sutures—although the clinician would normally put composite in each corner to maintain it and would not etch. Usually after 2 weeks, there is stability. Figure 15 shows the postoperative radiograph, and Figure 16 shows a radiograph 4.5 years later. The patient's probing went from 3 to 4 mm, but overall it was a success because something is always lost coronally, whether the case is a replant or an implant.
Post Diameter, Texture, and Material
Post diameter and texture are other important concerns. Achieving less than one-third of the diameter of the root is ideal, and at least a millimeter of dentin should be achieved circumferentially. Without that, the clinician would be looking for a fracture. One millimeter is the minimum, with one-and-a-half millimeters being ideal. With regard to texture, serrated and roughened posts provide greater retention because they provide more surface area. Similarly, the clinician can sandblast. Additionally, the cement that is used is important. Luting agents are not all equal. Resin and glass-ionomer cements are generally superior to others.9 Custom cast post and core is more prudent for use in large canals or very oval canals in some maxillary anterior teeth, such as No. 8, No. 9, and No. 10.
Prefabricated posts are better for circular canals and are less expensive, but there are definitely times where a clinician would want to do the cast and core, especially if they do not have a lot of tooth structure; it will be significantly better for the retention of the tooth.10 The canal diameter dictates the size of the post, not the root diameter. Sometimes with big oval canals, the post and core can spin around, especially on a cast post and core. Adding a keyway in the bulkiest part of the remaining tooth structure will help to resist rotational forces.
As to which material to use, the literature indicates fiber is better because it has greater flexibility and is less likely to allow for vertical fractures.2,3 It also has better esthetics, which is significant for both anterior and posterior teeth. The problem with fiber posts is that they can snap off and pull out. When they snap off, they are difficult to remove. A tapered diamond bur or ultrasonic can be used, but it must be done very carefully. Depending on the circumstances, metal can also be difficult, but metal is often serrated or threaded and can be unwound with an ultrasonic. However, fiber is significantly more flexible because it has a better modulus of elasticity, which should be as close to the dentin's elasticity as possible. On the radiograph, it can be difficult to see. Figure 17 shows a case with a good fiber post on the lateral that could be longer. The central should definitely be longer than it is. Because the clinician thought the posts and crowns were well done with good seals, when the patient had pain and apical radiolucencies, they were treated with apicoectomies. This was easier and less invasive than dismantling the previous structure.
Other Considerations
In deciding whether to use a post, the clinician must take the unique factors involved in each case into consideration. Figure 18 shows a case where the post was essentially useless and not congruent with the walls of the tooth. Figure 19 shows what the tooth looked like without the post. There was some decay, but the clinician was still able to save the tooth. Figure 20 shows the postoperative radiograph; Figure 21 was taken 6 months later. The clinician had told the patient that healing would need to be checked 6 months postoperatively to determine whether she could get a crown. There were two options for the tooth: (1) doing what the clinician did, which was to build internally as well as from mid-root with composite, or (2) use a fiber post. Several fiber posts could have been placed in the tooth as a better option, but this patient did not want to spend much and was unsure about the crown.
Another time when a post cannot be placed is when there is internal or external resorption. In the case shown in Figure 22, internal resorption occurred. Today it would be much easier to ascertain with CBCT. Here, the clinician filled the resorption with gutta-percha, and then above the gutta-percha, the mid-root coronal section was filled with composite. Because of how weakened the tooth was already, the clinician wanted to do whatever was possible to prevent it from weakening further. Figure 23 shows the postoperative radiograph, and Figure 24 shows the 2-year checkup. The only post that could be placed would have been a fiber post.
When considering cores, the clinician has many good options. Cores today are exceptional. The best quality core mimics the hardness of dentin. Clinicians must simply ensure that whatever they use to etch and bond is compatible with the core.
Finally, it is important to think in the 3-dimensional (3D). Most observers may believe the case in Figure 25 looks good, ignoring the root-canal access. From Figure 26, one can see that the situation actually is not ideal—about 20% may be filled, meaning that 100% is not clean. When viewing radiographs, it is common to consider them from the incomplete perspective shown in Figure 25. If a patient is experiencing sensitivity seemingly inexplicably, it may be useful to view the tooth in 3D with CBCT—the true dimensions of the tooth should be considered.
Conclusion
Techniques for placement of posts—or the equally important decision not to place a post—depend on the particular conditions of each unique case. The best option is to aim for the most conservative access, while determining whether a prefabricated or fiber post is ideal. Clinicians should adhere to post placement principles for retention of cores and strengthening of connections between coronal buildup material and tooth structure. Successful post and core considers quantity and quality of tooth structure, along with adjacent teeth, occlusion, parafunction, and future restorations. It also takes into account patient goals and reasonable possibilities for their budgets. In the end, providing the most optimal patient care is accomplished by careful decision-making before, during, and after root canals and other endodontic treatments.
About the Author
Joseph Chikvashvili, DDS
Private Practice
West Orange, New Jersey
References
1. Larson TD, Douglas WH, Geistfeld RE. Effect of prepared cavities on the strength of teeth. Oper Dent. 1981;6(1);2-5.
2. Mohan SM, Gowda EM, Shashidhar MP. Clinical evaluation of the fiber post and direct composite resin restoration for fixed single crowns on endodontically treated teeth. Med J Armed Forces India. 2015;71(3):259-264.
3. Adanir N, Belli S. Evaluation of different post lengths' effect on fracture resistance of a glass fiber post system. Eur J Dent. 2008; 2(1):23-28.
4. Cheung W. A review of the management of endodontically treated teeth. Post, core and the final restoration. J Am Dent Assoc. 2005;136(5):611-619.
5. Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63(5):529-536.
6. Hargreaves KM, Berman LH. Cohen's Pathways of the Pulp. 11th ed. Mosby; 2015.
7. Yu CY. Role of occlusion in endodontic management: report of two cases. Aust Endod J. 2004;30(3):110-115.
8. Rahimi S, Shahi S, Nezafati S, et al. In vitro comparison of three different lengths of remaining gutta-percha for establishment of apical seal after post-space preparation. J Oral Sci. 2008;50(4):435-439.
9. Ingle JI, Bakland LK. Endodontics. 5th ed. BC Decker; 2002.
10. Uniyal S, Aeran H, Kwatra B, Nautiyal A. Post & core: an easy and effective treatment modality for severely damaged teeth. International Journal of Oral Health Dentistry. 2015;1(2):99-104.