You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Before beginning complete denture treatment, it is critically important to determine if there are underlying problems during the pretreatment examination and diagnosis.1-3 The orofacial complex should be restored to an optimal state of health during the treatment planning stage. When this state of health is not obtained prior to prosthetic treatment, a therapeutically unacceptable end result is often the result.4 Although underlying problems are usually associated with long-term usage of ill-fitting dentures, they may also be present in patients who are in need of their first dentures.4 Problems associated with the fit, form, and function of old prostheses may require the dentist to either modify the existing prostheses, duplicate the existing prostheses and modify them, or make completely new treatment prostheses for the patient.4
Reduced VDO and PoorMandibular Posture
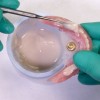
Residual ridge resorption and wear of the prosthetic teeth are noted to be the two major causative factors for lost vertical dimension of occlusion (VDO) in complete denture wearers.1,5-7 A reduced VDO may result in poorly conditioned tissues that are incapable of providing adequate support to the prosthesis. Other possible results of a reduced VDO include reduction of lower face height, compromised facial esthetics, an acquired Class III maxillomandibular relationship, angular cheilitis, and temporomandibular joint (TMJ) sounds on auscultation.8 Habitual mandibular posturing and altered neuromuscular programming in patients presenting with an insufficient VDO may cause difficulty in registering an accurate maxillomandibular relationship (Figure 1).9 Therefore, it is extremely important to reestablish an esthetically appropriate and functional VDO prior to the definitive therapy.9 Patients with a collapsed VDO may need to be reprogramed with an orthopedic device (which can maintain the mandible at an increased VDO) so that they can adapt to a new jaw separation position.1,9 It is important to improve the fit of the existing dentures and the health of the intraoral tissues before fabrication of the orthopedic device. A tissue conditioning material can be used to help restore the health of the denture bearing tissues (Figure 2).10
The orthopedic device can be fabricated by modifying the existing or duplicate complete dentures using the functionally generated path method and an intraoral gothic arch tracer (Massad jaw recorder, Nobilium).1,9 The first step in fabrication of the orthopedic occlusal device is determining the optimal VDO, which should be approximately 2 to 4 mm less than the vertical dimension at rest (VDR). VDR is recorded by first marking a dot on the tip of the patient's nose and another dot on the chin. Then, the patient is asked to take a deep breath and relax. When the patient is fully relaxed, a caliper or Boley gauge is used to record the distance between the two dots.1,9 The VDR measurement represents the patient's physiological rest position.
The intraoral gothic arch tracer is mounted on the dentures (Figure 3 and Figure 4). The striking plate is attached to the maxillary denture, and the pin with the pin receiver is attached to the mandibular denture. After the prostheses with the attached intraoral tracer assembly are placed in the patient's mouth, the patient is instructed to close slowly until the pin touches the striking plate. At this point, the VDO is evaluated, and the pin is adjusted vertically to ensure that the VDO is 2mm to 4mm less than the VDR. With the mandible in centric relation and the pin contacting the striking plate, the space between the opposing posterior occlusal surfaces is assessed. If adequate space is not available, the occlusal surfaces of the mandibular posterior denture teeth are adjusted using rotary instrumentation (Figure 5).
Next, the maxillary prosthetic teeth are lubricated (Vaseline, Unilever), and autopolymerizing tooth-colored acrylic resin (Palavit 55VS, Kulzer) is mixed and placed over the occlusal surfaces of the mandibular teeth (Figure 6). Until the acrylic resin has initially polymerized, the patient is asked to perform all of the mandibular movements (ie, right and left lateral and protrusive excursions) (Figure 7). Following initial polymerization, the mandibular denture containing the functionally generated orthopedic device is removed from the mouth and evaluated. It is placed in a polymerization pressure pot containing warm water and pressurized to 20 pounds/inch to eliminate the residual monomer.9 Upon removal, the device is finished and polished, and the denture is placed back in the patient's mouth. The orthopedic device aids in promoting functional and muscular harmony by establishing bilaterally balanced occlusal contacts with the desired vertical (ie, VDO) and horizontal (ie, centric relation) maxillomandibular relationships.9
Oral Hygiene
Poor oral hygiene promotes biofilm formation, which may result in soft-tissue inflammation.11 Furthermore, persistent inflammation accompanied by infection can cause deterioration of the osseous structures.11-13 Inflammation and infection in the location of natural teeth or dental implants can lead to periodontitis and loss of teeth or loss of osseointegration and failure of the implants, respectively.11,14,15In an edentulous patient, poor hygiene may lead to extreme traumatization and irritation of the denture bearing tissues.
The maintenance of appropriate hygiene for oral tissues and the prostheses helps maintain the overall oral health of the denture patient.16 Hygiene is a crucial factor that aids in promoting the long-term success of dentures.16 Poor oral and denture hygiene is usually attributed to a lack of patient motivation or awareness, the presence of complicated restorations, and/or poor dexterity (Figure 8).16 Patients' previous oral and denture hygiene habits can be an indicator of how they will comply with new dentures.3 Patients who demonstrate poor or nonexistent denture and oral hygiene should be educated, trained, and observed for a period of time. New prostheses should be fabricated only when the patient is exhibiting acceptable oral hygiene habits. The cameo surface contour and the decision to create surface characteristics such as diastema, festooning, and stippling should be influenced by the oral hygiene practices of the denture wearer, because these surface characteristics can make oral hygiene more challenging for those with limited dexterity or vision.
When an implant-retained overdenture is indicated, the type and design of the implant restoration selected should be informed by the patient's level of oral hygiene compliance.16 Removable restorations (both tooth-supported and implant-supported) are easily removed from the mouth and cleaned; therefore, they are indicated in patients who demonstrate poor oral hygiene.17 In addition, the selection of implant attachments should be chosen based on the oral hygiene compliance of the patient.18 For patients with poor oral hygiene compliance, freestanding attachments (eg, Locator®, Zest Dental Solutions; ERA®, Sterngold) are a preferred choice over those with connected bars.18
Denture Retention Factors
It is critical to evaluate the oral cavity for factors that may affect the retention of complete dentures. They include the following1:
Saliva quality. A decrease in salivary output will affect the retention of complete dentures and may cause generalized soreness in the denture bearing soft tissue due to frictional irritation.2 Saliva that is ropy, viscous, or mucinous has poor cohesive and adhesive properties that prohibit optimal denture retention. Patients should be informed about these conditions, educated regarding implications, and instructed about necessary treatment, including the use of denture adhesives, saliva substitutes, and implants for improving the prognosis.1
Arch size. Smaller sized arches (ie, < 35 mm width and < 45 mm anterior to posterior) offer inferior retention and stability when compared with larger arches (ie, > 45 mm width and > 55 mm anterior to posterior).1
Ridge height. Reduced residual ridge height has been found to adversely impact the potential for denture retention and stability.1
Cross-sectional form. Tall, V-shaped maxillary ridges with thin crests or extremely short to flat ridges are typically associated with relatively poor denture support, stability, and retention when compared with U-shaped ridges.1,3
Muscle attachments. Unfavorable location of the muscle and frenum attachments (ie, close to the ridge crest) will have a detrimental effect on the retention and stability of complete dentures. Frenum or muscle attachments located close to the ridge crest can be detrimental to the success of dentures and need to be corrected by preprosthetic surgery.1
Palatal vault. Tapered or V-shaped palatal vaults provide less stability when compared with square or rounded palatal vaults and can cause patient gagging due to the greater processing shrinkage associated with them.1
Palatal throat form. A narrow palatal throat form will have less tissue present for establishing the posterior palatal seal necessary for the retention of dentures.1,3
Patents affected by the abovementioned factors should be identified, educated, and offered implants to achieve optimal retention and stability of their dentures.
Unhealthy Denture Bearing Tissues
Continuous resorption and prosthetic tooth wear may lead to distortion of the surface contours of the residual ridge, which will ultimately result in poor tissue heath. Unhealthy or pathologic tissues are not able to withstand normal masticatory forces. Pathologic conditions worsen with the continuous use of dentures because they are accompanied by foreign bodies that further irritate the tissues. New dentures fabricated on abused or irritated tissues will exhibit reduced retention, lack of stability, and changing occlusal relationships.19 Therefore, the health and form of the denture supporting tissues must be optimized prior to the fabrication of new dentures. Tissue conditioning materials can be used to promote recovery of denture bearing soft tissues without having to ask patients to discontinue the use of their dentures.10
Prolonged usage of an old denture may lead to problems with flange extensions.4 Overextended flanges may result in tissue trauma (Figure 9). They must be relieved and adjusted appropriately, and the patient should be recalled regularly for evaluation.4 Prominent frenum attachments can prevent the development of an optimal border seal and may require surgical repositioning or removal.4 The presence of depressed irregularities, exostoses, tori, hypertrophic tuberosities, and significant undercut areas in the denture foundation should be noted. Surgical intervention should be considered for any defects expected to cause chronic soft tissue irritation, restrict normal function, prohibit optimal impression making, or interfere with proper denture border extensions (Figure 10).1,20,21
Additionally, enlarged tuberosities may affect the available vertical restorative space for the prostheses. The fabrication of prostheses within an inadequate restorative space can result in physiologically inappropriate contours, compromised structure and esthetics, encroachment upon the interocclusal rest space, and suboptimal retention and stability.22 When less than 3 mm of vertical restorative space is available for denture fabrication, surgical recontouring of any enlarged tuberosities should be considered (Figure 11).20-22
Retracted Tongue Position
Tongue position is important to maintain stability of the lower denture and develop the proper length of the lingual flange.23 Tongue positions may be classified as “normal” or “retracted” (Figure 12).23 A normally positioned tongue completely fills the floor of the mouth. The lateral borders rest over the posterior edentulous ridges, where they would normally rest over the occlusal surface of the posterior teeth, and the tip of the tongue rests on or is just lingual to the anterior ridge crest. This tongue position maintains the correct position of the floor of the mouth. Retracted tongue posture is demonstrated when the tongue is pulled back, exposing the floor of the mouth, and the lateral borders are either medial to or posterior to the edentulous ridge. In addition, the tip of the tongue is located in the posterior portion of the mouth or is withdrawn into the body of the tongue itself. Approximately 35% of patients present with retracted tongue posture.23 The prognosis of patients with a retracted tongue can be improved by making them aware of their condition and instructing them to position the tongue correctly during rest and function. Prescribing tongue exercises23 and placing a training bead of resin on the lingual aspect of the denture in between the central incisors24 can also help retrain the tongue and maintain its proper position (Figure 13 and Figure 14).
Nutrition
It is critical to assess the nutritional intake and overall physical and mental health of edentulous patients, especially those who are elderly. General health and the health of the denture bearing tissues are greatly impacted by nutritional intake (Figure 15). Some oral lesions may be diagnosed by evaluating the patient's nutritional intake. These can be easily differentiated from those resulting from other causes by a rapid reversion to normal following appropriate dietary and supplement therapy. Poor nutritional intake in an elderly individual may be due to a physiological reason, a mental health issue, or a sequela of an ill-fitting prosthesis.25
Patients should be advised regarding the importance of a balanced diet.26 They should be encouraged to eat a variety of foods, including protein sources, dairy products, fruits, vegetables, grains, and cereals; to consume water, fresh fruit juices, and milk; and to limit the intake of salt, fat, and sugar.26-28 Dietary guidance and nutritional care should be an integral part of the prosthodontic treatment of the edentulous patient.6
Joint Disorders
TMJ disorders are prevalent among complete denture wearers.29-31 Prolonged use of old dentures, psychological and emotional factors associated with increasing age, and loss of natural dentition may lead to increased TMJ disorders in edentulous patients.30,32-34 These disorders can result in changing occlusal relationships, pain, patient discomfort, reduced mouth opening, deviation of the mandible upon opening, and poor adaptation to the new prostheses. In edentulous patients, less than 60 mm is considered a reduced mouth opening. Because TMJ disorders may be the cause of ongoing occlusal problems among denture patients, it is important to resolve any pain and rehabilitate the TMJs to a healthful state before the fabrication of new prostheses is attempted.35
Conclusion
Failure to resolve common conditions affecting the orofacial complex and rehabilitate it to a dependable, healthy level may result in the failure of denture prostheses. To help ensure a successful outcome, a thorough clinical examination, which assesses VDO, mandibular posture, oral hygiene, the health and retentiveness of denture bearing tissues, tongue position, nutrition, and potential TMJ disorders, should be performed and any issues treated prior to commencing prosthetic treatment.
About the Authors
Russell A. Wicks, DDS, MS
Professor and Chairman
Department of Prosthodontics
University of TennesseeHealth Science Center
College of Dentistry
Memphis, Tennessee
Joseph J. Massad, DDS
Associate Professor
Department of Prosthodontics,
University of TennesseeHealth Science Center
College of Dentistry
Memphis, Tennessee
Swati A. Ahuja, BDS, MDS
Adjunct Assistant Professor
Department of Prosthodontics
University of TennesseeHealth Science Center
College of Dentistry
Memphis, Tennessee
Charles J. Goodacre, DDS, MSD
Distinguished Professor
Loma Linda University
School of Dentistry
Loma Linda, California
References
1. Massad J, Cagna DR, Goodacre CJ, Wicks R, Ahuja SA. (2017). Application of the Neutral Zone in Prosthodontics. Hoboken, NJ: John Wiley and sons, Inc.; 2007:1-33.
2. Barone JV. Diagnosis and prognosis in complete denture prosthesis. J Prosthet Dent. 1964;14:207-213.
3. House MM. The relationship of oral examination to dental diagnosis. J Prosthet Dent. 1958;8:208-219.
4. McCord JF, Grant AA. Pre-definitive treatment: rehabilitation prostheses. Br Dent J. 2000; 188(8):419-424.
5. Ismail YH, George WA, Sassouni V, et al. Cephalometric study of the changes occurring in the face height following prosthetic treatment. I. Gradual reduction of both occlusal and rest face heights. J Prosthet Dent. 1968;19(4):321-330.
6. Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 years. J Prosthet Dent. 2003;89(5):427-435.
7. Tallgren A, Lang BR, Walker GF, et al. Roentgen cephalometric analysis of ridge resorption and changes in jaw and occlusal relationships in immediate complete denture wearers. J Oral Rehabil. 1980;7(1):77-94.
8. Wagner AG. Complete dentures with an acquired protrusive occlusion. Gen Dent. 1989;37:56-57.
9. Massad JJ, Connelly ME, Rudd KD, et al. Occlusal device for diagnostic evaluation of maxillomandibular relationships in edentulous patients: a clinical technique. J Prosthet Dent. 2004;91(6):586-590.
10. Gonzalez JB. Use of tissue conditioners and resilient liners. Dent Clin North Am. 1977;21(2):249-259.
11. Cagna DR, Massad JJ, Daher T. Use of a powered toothbrush for hygiene of edentulous implant-supported prostheses. Compend Contin Educ Dent. 2011;32(4):84-88.
12. Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29(Suppl 3):197-212.
13. Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998;17:63-76.
14. Leonhardt A, Dahlén G, Renvert S. Five-year clinical, microbiological, and radiological outcome following treatment of peri-implantitis in man. J Periodontol. 2003;74(10):1415-1422.
15. Quirynen M, De Soete M, van Steenberghe D. Infectious risks for oral implants: a review of the literature. Clin Oral Implants Res. 2002;13:1-19.
16. Ahuja S, Wicks R, Selecman A. Fabrication of new restorations with a consideration of oral hygiene. J Indian Prosthodont Soc. 2016;16(3):307-310.
17. DeBoer J. Edentulous implants: overdenture versus fixed. J Prosthet Dent. 1993;69(4):386-390.
18. Massad JJ, Ahuja S, Cagna D. Implant overdentures: selections for attachment systems. Dent Today. 2013;32(2):128-132
19. Lytle RB. The management of abused oral tissues in complete denture construction. J Prosthet Dent. 1957;7:27-42.
20. Yrastorza JA. Surgical problems in edentulous jaws associated with denture construction: a review. J Oral Surg Anesth Hosp Dent Serv. 1963;21:202-209.
21. Kelly EK. The prosthodontist, the oral surgeon, and the denture-supporting tissues. J Prosthet Dent. 1966;16(3):464-478.
22. Ahuja S, Cagna DR. Classification and management of restorative space in edentulous implant overdenture patients. J Prosthet Dent. 2011;105(5):332-337.
23. Wright, CR. Evaluation of the factors necessary to develop stability in mandibular dentures. J Prosthet Dent. 2004;92(6):509-518.
24. Kuebker WA. Denture problems: causes, diagnostic procedures, and clinical treatment. I. Retention problems. Quintessence Int Dent Dig. 1984;15(1):1031-1044.
25. Bandodkar KA, Aras M. Nutrition for geriatric denture patients. J Indian Prosthodont Soc. 2006;6(1): 22-28.
26. Rathee M, Hooda A. Nutritional status in denture wearers: A review. The Internet Journal of Nutrition and Wellness. 2009;10(2):1-5.
27. Norlén P, Steen B, Birkhed D, et al. On the relations between dietary habits, nutrients, and oral health in women at the age of retirement. Acta Odontol Scand. 1993;51(5): 277-284.
28. Chauncey HH, Muench ME, Kapur KK, et al. The effect of the loss of teeth on diet and nutrition. Int Dent J. 1984;34(2):98-104.
29. Alzarea BK. Temporomandibular disorders (TMD) in edentulous patients: a review and proposed classification (Dr. Bader's classification). J Clin Diag Res. 2015;9(4):ZE06-ZE09.
30. Sakurai K, San Giacomo T, Arbee NS, Yukstas AAA. A survey of temporomandibular joint dysfunction in completely edentulous patients. J Prosthet Dent. 1988;59(1):81-85.
31. Zissis AJ, Karakazis HC, Polyzois GL. The prevalence of temporomandibular joint dysfunction among patients wearing complete dentures. Aus Dent J. 1988;33(4):299-302.
32. Al-Shumailan YR, Al-Manaseer WA. Tempo-romandibular disorder features in complete denture patients versus patients with natural teeth; A comparative study. Pakistan Oral and Dentat Journal. 2010;30(1):254-259.
33. Tzakis MG, Osterberg T, Carlsson GE. A study of some masticatory functions in 90-year-old subjects. Gerodontololgy. 1994;11(1):25-29.
34. Shet RG, Rao S, Patel R, et al. Prevalence of temporomandibular joint dysfunction and its signs among the partially edentulous patients in a village of North Gujarat. J Contemp Dent Pract. 2013;14(6):
1151-1155.
35. McHorris, WH. TMJ dysfunction - Resolution before reconstruction. J Eur Acad Gnathol. 1974;1:16-32.