You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
A new approach to replacement of the four mandibular incisors is proposed in this clinical report. The four mandibular incisors are the teeth most frequently lost because of periodontal disease.1,2 Their replacement with immediately placed implants and a nonocclusally loaded provisional restoration is a simple, predictable, and minimally invasive procedure.
This approach compares favorably with conventional therapies in several aspects. Typically these teeth are extracted and replaced with either a tooth-borne or implant-supported fixed partial denture, or a removable partial denture. The interim treatment options commonly considered are a transitional removable partial denture, a resin-bonded fixed provisional restoration, or a conventional fixed provisional restoration using full-coverage crown preparations of the adjacent cuspids. The interim management of these cases in any of these three conventional ways poses difficulties for the patient and clinician and can complicate the final treatment outcome.
A transitional removable partial denture placed over healing extraction sites may be cumbersome and uncomfortable for the patient. It may cause pressure on the tissues and/or graft (if necessary), thereby resulting in compromised healing or failure of a graft. Resin-bonded provisional-fixed restorations can protect extraction sites but are generally used without preparation of the abutment teeth. Therefore, these restorations may not be retentive over an extended period. Postsurgically, as the tissue heals and the ridge recontours, the clinician must be able to make alterations of the tissue surface of the provisional restoration. This becomes difficult to manage with the resin-bonded restorations, which would have to be removed and rebonded repeatedly. Furthermore, if the cuspids have been previously restored with full-coverage restorations that do not require replacement, the bonded-bridge option is precluded. The third treatment alternative, a conventional six-unit full-coverage fixed provisional restoration from cuspid to cuspid, would require the preparation of both cuspids solely for the purpose of interim management. It is accepted that unnecessary sacrifice of healthy tooth structure should be avoided.
Materials and Methods
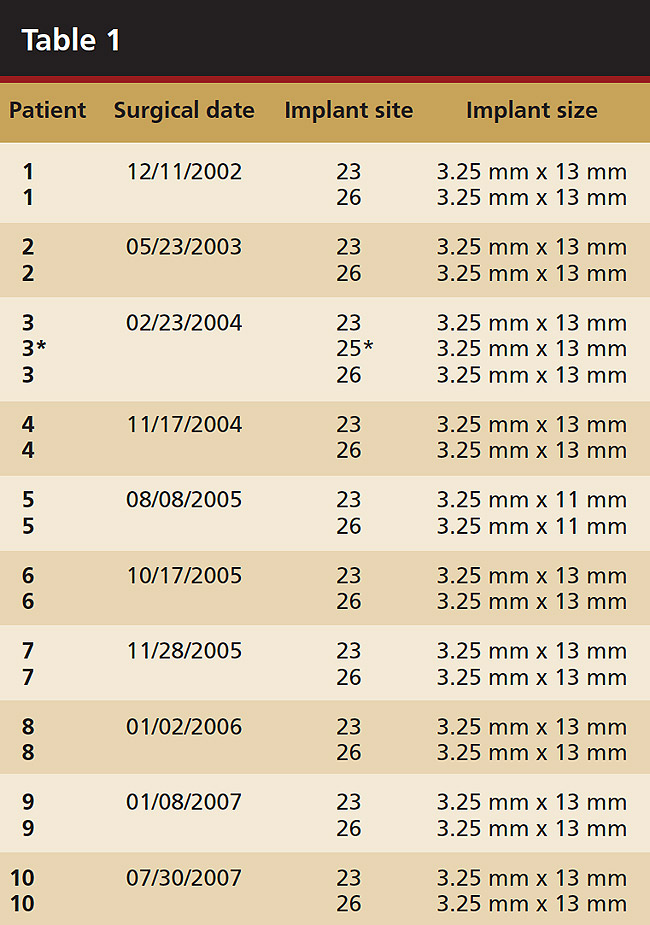
A total of 10 consecutive cases that were scheduled to lose the four mandibular incisors because of localized severe periodontal disease were documented. There were 21 implants immediately placed and temporized with nonocclusally loaded provisional restorations (Table 1). All cases were restored with screw-retained provisional and, subsequently, permanent restorations.
 |
Case Report and Technique
A 53-year-old male presented with localized advanced periodontal disease of the mandibular incisors. Teeth Nos. 23 to 26 exhibited Class II mobility because of advanced bone loss (Figure 1). The teeth had migrated out of position over the years, and a diastema had developed between No. 24 and No. 25 (Figure 2). The patient complained about the poor esthetic appearance of these teeth, and he was able to perceive their loss of strength on function as a result of their mobility.
Treatment alternatives that were discussed included a removable partial denture, a resin-bonded bridge, a conventional fixed partial denture including the cuspids, and an implant-supported fixed partial denture. The patient did not want a removable prosthesis, interim, or otherwise. His cuspids were in good condition and required no restorative treatment.
Radiographic and clinical examination determined there was a sufficient volume of bone for implant placement. The facial walls of bone were intact. The patient was advised extractions and immediate placement of two implants with a nonocclusally loaded provisional restoration would be the treatment of choice. The patient understood at the time of extraction and implant placement that if the stability of one or both implants was not sufficient for immediate loading, he would have no choice but to accept a removable or bonded interim provisional restoration. He was informed that his postoperative instructions would include a diet of soft foods only for the first 6 to 8 weeks following surgery.
Preoperatively, 1 g of amoxicillin was administered. Using local anesthesia (lidocaine 1:100,000 epinephrine), extractions of teeth No. 23 to No. 26 were performed without raising a flap and with gentle luxation to preserve the remaining facial osseous plate. The sockets were curetted prior to implant placement. A vacuum-formed surgical guide, fabricated based on a diagnostic wax-up of the desired tooth positions for the subsequent fixed prosthesis, was used during implant placement. Osteotomies were performed at sites No. 23 and No. 26 and positioned toward the lingual aspects of the sockets (Figure 3A and Figure 3B). Two tapered implants (OsseoTite™ 313, BIOMET 3i™, Palm Beach Gardens, FL) measuring 3.25 mm x 13 mm were placed. Conical prosthetic abutments (3-mm height) were used to facilitate joining the two implants in a screw-retained fixed partial denture (Figure 4). A laboratory-processed acrylic-resin provisional restoration was altered to allow connection to the temporary cylinders. The provisional was placed into the vacuum-formed surgical guide that was now used to maintain the provisional in the correct 3-dimensional position (Figure 5) while being attached to the temporary cylinders with acrylic resin intraorally. Once a sufficient amount of acrylic resin was placed to secure the cylinders to the provisional, it was removed from the mouth and its contours were completed at the laboratory bench (Figure 6A). The two central incisor sockets were grafted with small-particle allograft material (Puros® Allograft, Zimmer Dental, Carlsbad, CA) to maintain gingival architecture beneath two ovate pontics (Figure 6B). The provisional restoration was inserted and the screws tightened to 20 Nt-cm of torque.
The patient was given postoperative instructions and advised to maintain a soft diet for 6 to 8 weeks to protect the implants. The patient was followed weekly for the first 3 weeks and monthly thereafter. After 4 months of healing, the provisional restoration was removed and the soft tissues were examined. Mature, keratinized gingival tissues were present facially, lingually, and interproximally. Nonkeratinized tissue could be seen at the tissue surfaces of the ovate pontics and in the intrasulcular regions of the implant abutment units. No clinical probing depths beyond 1 mm were found adjacent to the abutments. The healed tissue represented an acceptable clinical result especially in light of the gap that had been present at the time of implant placement (Figure 7A and Figure 7B). Final impressions were made, and the permanent ceramo-metal screw-retained prosthesis was placed within 8 weeks (Figure 8).
This patient has been followed for 4 years with no complications and no discernable clinical changes in soft- or hard-tissue levels.
Results
The patients have been followed for up to 6 years with an implant survival rate of 100%. No clinical problems have arisen.
Discussion
Single-tooth replacement with an immediate implant and a nonocclusally loaded provisional restoration has been described in the literature as an effective and predictable treatment option with implant survival rates similar or equal to that of implants placed in a delayed protocol (98% to 100%).3,4 It has also been shown that one can expect an unpredictable degree of bone and soft-tissue remodeling and recession at the facial aspect of the immediately placed implant.5 Placement of the implant against the bony wall of the extraction socket does not enhance preservation of the facial crest of bone.6 Therefore, in the esthetic zone, one must be aware of the difference between the predictably high implant survival rates and the somewhat less consistent esthetic success rate. If the implant survives but the soft tissue remodels and recession ensues, the implant restoration may be considered a failure. Patient selection is paramount in immediate implant cases, and the patient must be made aware of the potential esthetic compromises.
The efficacy of immediate implants with nonocclusally loaded provisional restorations in partially edentulous jaws has been supported by numerous studies and it is an accepted treatment option in many clinical situations.7-14 The survival rate of immediately loaded implants placed in periodontally susceptible patients has also been shown to be similar to that of nonsusceptible patients.15
The anterior mandible is a favorable site for immediate implants and provisional restorations for several reasons: the bone quantity and quality are most often adequate for predictable implant placement; the tooth sockets are usually narrower (mesio-distally) and shorter than the subsequent osteotomy so that the implants may be stabilized by bone beyond the sockets; and of the four tooth positions in the anterior mandibular, only two need to be used for implant placement. The implants can be placed in either the central or lateral positions on both the left and right sides. In the anterior mandible, there is no potential for intraoperative nerve damage because the inferior alveolar nerve does not course through the mandible between the mental foramina. Given that this area is not commonly in the patient’s perceived esthetic zone, a small amount of gingival recession that may occur following healing16,17 may be acceptable. If the cuspids are periodontally sound and retained intact (without any tooth preparation), they will protect the newly placed implants and provisional restoration from excessive occlusal forces.18 The patient must be instructed to use caution when eating to avoid biting with the immediate provisional restoration in the anterior mandible for the first 6 weeks.
Conclusion
The evidence in the literature, along with this report of 10 consecutive clinical cases, supports the concept that replacing the four mandibular incisors with two immediate implants and an immediate nonocclusally loaded fixed-provisional restoration may be the most predictable, least invasive option available. This should lead to a shift in treatment planning approach and may now be considered the optimal treatment choice for most patients requiring the replacement of the four mandibular incisors. More research is needed with a larger number of patients to verify the results of these 10 consecutive cases.
References
1. Baqain ZH, Khraisat A, Sawair F, et al. Dental extraction for patients presenting at oral surgery student clinic. Compend Contin Educ Dent. 2007;28(3):146-150.
2. McCaul LK, Jenkins WM, Kay EJ. The reasons for the extraction of various tooth types in Scotland: a 15-year follow up. J Dent. 2001; 29(6):401-407.
3. Wöhrle P. Single-Tooth Replacement in the aesthetic zone with immediate provisionalization: fourteen consecutive case reports. Pract Periodontics Aesthet Dent.1998;10(9):1107-1114.
4. Grunder U, Polizzi G, Goené R, et al. A 3-year prospective multicenter follow-up report on the immediate and delayed-immediate placement of implants. Int J Oral Maxillofac Implants.1999;14(2):210-216.
5. Covani U, Cornelini R, Barone A. Bucco-lingual remodeling around implants placed into immediate extraction sockets: a case series. J Perio-dontol. 2003;74(2):268-273.
6. Araújo MG, Lindhe J. Dimension ridge alternations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005; 32:212-218.
7. Testori T, Galli F, Capelli M, et al. Immediate nonocclusal versus early loading of dental implants in partially edentulous patients: 1-year results from a multicenter, randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2007;22(5):815-822.
8. Jaffin RA, Kumar A, Berman CL. Immediate loading of implants in partially and fully edentulous jaws: a series of 27 case reports. J Perio-dontol. 2000;71(5):833-838.
9. Testori T, Bianchi F, Del Fabbro M, et al. Immediate non-occlusal loading vs. early loading in partially edentulous patients. Pract Proced Aesthet Dent. 2003;15(10):787-794.
10. Ganeles J, Wismeijer D. Early and immediately loaded dental implants for single-tooth and partial-arch applications. Int J Oral Maxillofac Implants. 2004;19(suppl):92-102.
11. Crespi R, Capparè P, Gherlone E, et al. Immediate occlusal loading of implants in fresh sockets after tooth extraction. Int J Oral Maxillofac Implants. 2007;22(6):955-962.
12. Esposito M, Grusovin MG, Willings M, et al. The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2007;22(6):893-904.
13. Guida L, Iezzi G, Annunziata M, et al. Immediate placement and loading of dental implants: a human histologic case report. J Periodontol. 2008;79(3):575-581.
14. Ostman PO, Hellman M, Sennerby L. Immediate occlusal loading of implants in the partially edentate mandible: a prospective 1-year radiographic and 4-year clinical study. Int J Oral Maxillofac Implants. 2008;23(2):315-322.
15. Macheti EE, Frankenthal S, Blumenfeld I, et al. Dental implants for immediate fixed restoration of partially edentulous patients: a 1-year prospective pilot clinical trial in periodontally susceptible patients. J Periodontol. 2007;78(7):1188-1194.
16. Covani U, Cornelini R, Barone A. Bucco-lingual remodeling around implants placed into immediate extraction sockets: a case series. J Periodontol. 2003;74(2):268-273.
17. Wöhrle, PS. Single tooth replacement in the aesthetic zone with immediate provisionalization: fourteen consecutive cases. Pract Periodontics Aesthet Dent. 1998;10(9):1107-1114.
18. Misch CE, Wang HL, Misch CM, et al. Rationale for the application of immediate load in implant dentistry: part II. Implant Dent. 2004; 13(4):310-321.
About the Authors
Richard B. Smith, DDS; Clinical Associate Professor, Department of Periodontology and Implant Dentistry, Post-Graduate Division, New York University College of Dentistry; Private Practice, New York, New York
Dennis P. Tarnow, DDS; Professor and Chair, Department of Periodontology and Implant Dentistry, Post-Graduate Division, New York University College of Dentistry; Private Practice, New York, New York
Marion Brown, DMD; Private Practice, New York, New York, New York University College of Dentistry; Private Practice, New York, New York
Jonathan Zamzok, DMD; Clinical Associate Professor, New York University College of Dentistry, Department of Periodontology and Implant Dentistry, Post-Graduate Division, New York University College of Dentistry; Private Practice, New York, New York











