You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
More than 50% of the general population has oral malodor,1 commonly known as “bad breath.” Present-day research has shown sulfur-producing anaerobic bacteria on the tongue form certain volatile organic compounds (VOCs) that produce unpleasant odors in the mouth. Numerous methods are used for assessing oral malodor severity. Traditional oral malodor assessment methods include organoleptic measurements and gas chromatography, while advanced technology has given rise to machines that make diagnosing oral malodor in dental clinics more convenient.
Diagnosis is only the first step in treatment. On consultation by dental professionals, patients must take further action to control and manage oral malodor in their daily lives. They can accomplish this either mechanically or chemically. Each case is treated differently, depending on its origin. By having a holistic grasp of where oral malodor originates and how to analyze and treat it, future dental products can be made to better cater to these patients. The consequences of having oral malodor are twofold. Oral malodor not only makes the individual feel uncomfortable in public places but also can be an indication of the individual’s overall well-being. Thus, careful analysis of oral malodor can be used as an approach in diagnosing systemic diseases and understanding how lifestyle habits affect oral health.
Oral and Non-Oral Causes
Oral malodor can be grouped into two categories: non-pathologic and pathologic, or chronic oral malodor. Non-pathologic oral malodor is temporary and caused by normal metabolic functions in the body. Causes may include the lack of proper salivary flow during sleep, hunger, food debris, smoking, and the use of prescription drugs.1 Substances absorbed into the circulatory system may be released in pulmonary air or saliva as volatile odoriferous compounds derived from foods.
Pathologic, or chronic oral malodor, can originate from oral causes, which are much more common than non-oral causes. Oral factors include poor dental hygiene, food particles in the teeth, periodontal disease, coating on the tongue, wearing dentures overnight, dry mouth, and defective restorations. Mucositis induced by radiation therapy exposure also could cause oral malodor. Other oral causes include Sjögren’s syndrome, peritonsillar abscess, cleft lip or palate, cancer of the pharynx, and cryptic tonsils.1
Pathologic oral malodor also can originate from non-oral causes, which include diabetic ketosis and acidosis; uremia; erratic bowel movement and regurgitations; hepatic and renal failure; and certain types of cancer, such as leukemia. Although select patients with a history of gastrointestinal diseases have experienced oral malodor, it has not been determined whether gastrointestinal diseases actually cause oral malodor. Furthermore, a few deviant physiologic processes, such as enzymatic and transport abnormalities (eg, trimethylaminuria), also may initiate oral malodor.
Saliva
Saliva plays a central role in the formation of oral malodor. One of the functions of saliva is to purge any remaining food debris from the oral cavity. Periodontal pockets can cause food debris to accumulate and the rate of foul-odor production to increase.2 Some medications may cause xerostomia and result in oral malodor, especially those with anticholinergic activity. Such medications include antihistamines (eg, astemizole, brompheniramine), tricyclic antidepressants (eg, amitriptyline, desipramine), diuretics (eg, chlorothiazide, furosemide), antihypertensives (eg, captopril, clonidine), and analgesics (eg, codeine, meperidine) (Table 1A and Table 1B).3 Sympatholytics also can cause xerostomia. They include α-blockers (eg, terazosin), α-2 agonists (eg, clonidine), and ß-blockers (eg, metoprolol).4 Oxazepam, which is a muscle relaxant and sedative, has side effects that include xerostomia; however, this is temporary.5
By studying incubated saliva, researchers can help determine how oral malodor and other oral developments are formed through the interaction of microbial flora in the mouth. Whole saliva is centrifuged and incubated in an aerobic environment. The incubation gives rise to a salivary sediment malodor system that represents the formation of oral malodor.6
The Tongue Plaque Coating
Through research,7 VOCs have been found to be the primary culprit of engendering oral malodor. VOCs are gaseous substances that are produced primarily on the tongue and contain volatile sulfur compounds (VSCs) hydrogen sulfide (H2S), dimethyl sulfide ([CH3]2S), methyl mercaptan (CH3SH), and sulfur dioxide (SO2). Oral malodor is created primarily on the tongue, with the VSCs made on the lingual dorsum. The bacteria that produce these VSCs can be found by evaluating biofilm and scraped specimens from the lingual dorsum, gingival pockets, and tonsillar crypts.7 VSCs are produced by gram-negative anaerobic bacteria that live on the lingual dorsum.8 These bacteria can thrive on the tongue because food debris accumulates rapidly on the tongue’s large surface area and papillae.
In a study by Tyrell et al,9 tongue samples were cultured and numerous bacterial species isolated. Among those isolated, the most common were Peptostreptococcus anaerobius, Collinsella aerofaciens, Eubacterium group, Actinomyces species, Eikenella corrodens, Veillonella species, Fusobacterium nucleatum, pigmented Prevotella species, and Selenomonas species. Other bacteria frequently found on the lingual dorsum were Treponema denticola, Porphyromonas gingivalis, Peptostreptococcus micros, Actinomyces israelli, Selenomonas flueggei, and Proteus mirabilis (Table 2). Tongue cleaning improves taste sensation and seems to reduce the substrata for putrefaction, rather than the bacterial load.10 The tongue coating consists of blood components, nutrients, epithelial cells, and bacteria. The amount of VSCs on the tongue is correlated with the amount of tongue coating. In addition to the VSCs, the presence of tongue coating may be related to the level of secretory immunoglobulin A (IgA) in the saliva. In patients who have only slight tongue coating, the concentration of secretory IgA was found to be higher than in patients with moderate-to-heavy coating. Combined with findings on Streptococcus species, secretory IgA may act as shielded protection against tongue plaque.11
Hess et al12 proposed a mathematical model to determine oral malodor formation. It describes the structure of the biofilm, transfer of oxygen, flow of substrates, and formation of VSCs, which are all part of the oral malodor process. According to this model, each papilla is a cluster of strands protruding perpendicularly from the tongue. The biofilm covers the core tissue of the papillae. The deeper layer of the biofilm is assumed to be anaerobic, while the superficial layer of the biofilm is considered aerobic. The biofilm metabolizes oxygen gradually. The only part of the papilla that is oxygenated is the upper tip, so aerobic bacteria can grow. Substrates can enter from above or below the biofilm. All of the substrates are converted to VSCs via a chain process. However, substrates that enter from above the biofilm are transient and soon depleted, while permanent substrates entering from below the biofilm become the source of oral malodor. VSCs leave the biofilm via four transport mechanisms: diffusion, conversion, salivary flow, and volatilization.
Microbiota-Associated Oral Malodor
Research has shown antibacterial agents can reduce oral malodor, supporting the idea that oral malodor has a bacterial origin.7 Gram-negative bacteria are the primary source of the malodor; however, gram-positive oral microorganisms play the initial role of producing such odors by facilitating proteolysis of certain amino acids pertinent to odor production. Although it was previously thought that gram-positive bacteria did not play a role in oral malodor, recent research has shown when antibacterial agents were used on gram-positive bacteria, mainly streptococci, there was a reduction in oral malodor in an in vitro model. Gram-positive bacteria species, such as Streptococcus salivarius deglycosylates (salivary glycoproteins), expose their protein core to be further degraded by gram-negative bacteria.7 Gram-negative bacteria produce odors in the presence of three amino acids. Reduction of methionine to methyl mercaptan and cysteine leads to the reduction of cysteine to cystine, which produces hydrogen sulfide when sulfhydrase-positive microbes are present.1,7 Recent research has shown VOCs, mainly alkanes or alkane derivatives played a significant role in oral malodor. These compounds are produced from high oxidative stress, which can be an indication of periodontal infection in the oral cavity. The VOCs, such as VSCs, are considered the most influential components of oral malodor.13
Oral Malodor Assessment Parameters
Organoleptic Measurements
Organoleptic measurements are considered to be the gold standard for measuring and assessing bad breath,14 which can be quantified based on the intensity of the odor and offensiveness. Organopleptic judges are trained before rating the subjects, using a four-phase training protocol based on the American Society of Testing and Materials standards. First, the organoleptic judges are introduced to the scales and sniffing techniques. Then, they perform exercises that consist of smelling pleasant, neutral, and unpleasant odors; identifying the odorant; and discriminating the odors from similar ones. Finally, the judges are assessed on how well they are trained, based on a post-test in which the same odorants used in pre-training were placed in a different order.15 There are gender and age differences in the judges’ performances, in which women have better performance and older individuals have lower performance.1 These judges independently rate the intensity of the odor in participants by the Rosenberg scale from 0 to 5, which is as follows: 0 = no odor; 1 = barely noticeable odor; 2 = slight but clearly noticeable odor; 3 = moderate odor; 4 = strong offensive odor; and 5 = extremely foul odor; with a score ≥ 2 equaling halitosis.1,15,16 The offensiveness of the odor is measured on a hedonic scale in which a score of +2 = like very much; +1 = like; 0 = do not like or dislike; -1 = dislike; and -2 = dislike very much.15 Many other hedonic scales are available with differing intensity ranges that are used in studies of oral malodor, with some scales being more common than others. Participants are asked to refrain from eating, using dental products, and/or wearing any type of perfume for 4 hours before the visits because these actions may affect the results.1,16
Portable Sulfide Meter
A portable sulfide meter has been used to test oral malodor because of its reproducibility and ease of use.1,16 Before the examination, participants are to refrain from all oral-related activities and wearing of fragrances that may influence the results, based on the sensitivity of the machine. They are asked to exhale for 30 seconds through a tube connected to the machine. The sulfide meter records a score based on VSC levels in parts per billion (ppb) based on electrochemic and voltametric sensors. There are three categories of scores: Normal = 80 ppb to 160 ppb; Weak = 160 ppb to 250 ppb; and Strong = > 250 ppb. “Weak” signifies malodor at a close distance, and “Strong” signifies malodor at a greater distance.16 This method is repeated three times, and the mean of the scores is taken.1,16 However, one major disadvantage of using this instrument is that it does not differentiate the various sulfide-containing compounds; for example, CH3SH is three times more unpleasant than H2S.1,2 Because of this limitation, the sulfide meter may underestimate oral malodor in patients who have higher CH3SH concentrations.2
Gas Chromatography
Gas chromatography (GC) is a highly reliable, objective, and reproducible technique for detecting oral malodor.14 GC measures the amount and type of specific VSC and VOCs in the mouth air. Samples of oral cavity breath are collected in a multi-laminate bag. The VOCs are extracted from breath samples onto sorbant traps. GC uses a flame photometric detector to analyze the odors. VOCs are identified by computer-based libraries and quantified by their amounts compared with an internal standard. Background VOC contaminants are quantified by inflating the sample bags with helium and subtracted from the VOCs in the breath.13 Although extremely precise, this method is not used commonly in chairside clinical settings because it takes a long time to run, is expensive, and requires a skilled operator.14,17 This method of measurement is particularly useful if the sample population is small.17
Portable Gas Chromatography
A portable GC device can be used to measure the VSCs in the breath18 and can identify oral malodor’s three causal components, which are hydrogen sulfide, methyl mercaptan, and dimethyl sulfide. The device also gives precise measurements of the concentrations of the compounds. To measure these concentrations in patients, a syringe (without the needle) is placed deep into the oral cavity. Then, the plunger is slowly withdrawn, inserted, and withdrawn again before the syringe is removed from the mouth. Then, the sample is injected into the machine where measurements start automatically. The benefits are its cost-effectiveness and convenience and is less time-consuming than traditional GC methods and, therefore, could be used readily in an office.18
Electronic Nose
The electronic nose is a handheld instrument that has the ability to “smell” and produce unique fingerprints for odors.1 One odor discrimination analyzer (electronic nose) has a chemical sensor system that uses six metal oxide semiconductor sensors for odor discrimination.1,19 Each sensor has to be selected based on the sensitivity and fragrance of the odorant being tested because of various pattern recognition software. To use an electronic nose, the mouth-air gas from a patient is first trapped in a tube for 30 seconds and then driven up a sensor section with pure nitrogen. An estimated VSC concentration and organoleptic score is calculated.19 This instrument has made odor analysis fast and simple and also is fairly cost-effective. Although the electronic nose has been used throughout the medical fields, few studies have been done to assess its effectiveness in clinically assessing oral malodor.1,19
Oral Malodor Management
For the general case of non-systemic oral malodor, treatment often begins with proper oral hygiene at home, in which the patient must brush, floss, and tongue scrape properly and regularly. These procedures will reduce the amount of VOCs and microorganisms in the mouth.20 Specifically, much emphasis has been placed on tongue cleaning to reduce the amount of coating on the back of the tongue. A recent study examined how different tongue-cleaning methods affected bacteria on the dorsal surface of the tongue for 4 days.21 After accessing 19 patients, researchers determined the most significant reductions in gram-negative bacteria were seen when toothbrushing was followed by tongue cleaning using a high-speed vacuum ejector and irrigating with mouthwash; this was the most inclusive of the procedures. Toothbrushing and tongue scraping was next in reducing tongue microflora, and toothbrushing alone demonstrated the least reduction.21 However, tongue scraping was shown to have a prolonged effect even on Day 4, whereas the other two mechanisms had temporary effects only. Thus, regular tongue cleaning is essential for providing long-lasting or overnight hindrance of bacterial formation.21 Because patients usually neglect tongue cleaning in daily oral hygiene as a result of discomfort or lack of familiarity with the practice, professionals should demonstrate the appropriate use of tongue scrapers.1 Then, patients can perform the action at home comfortably and effectively. Patients should start scraping as far back as possible to remove the most debris. Often, first-time tongue-scrapers will experience a gag reflex; however, they should be informed that this will subside eventually as they continue daily tongue cleaning. Tongue scrapers come in a wide variety: flexible metals or plastics, blunt flat edges or serrations, manual or electric, etc. Some are in vertical form, in which a handle and scraper are on the end. Patients should seek a scraper according to their preferences and needs.
In addition to mechanical means, products with antimicrobial components should be recommended to patients for use at home, such as mouthwashes containing cetylpyridinium chloride, chlorhexidine, triclosan, quaternary ammonium compounds, benzalkonium chloride hydrogen peroxide, sodium bicarbonate, zinc salts, or essential oils.1 These mouthwashes are formulated based on scientific evidence that they target microbiota on the tongue while maintaining the natural internal balance of the mouth.1 Such products may either reduce the concentration of VOCs and odor-causing microbes or act as oxidizing agents1 to neutralize the pH of the mouth to prevent growth of unwanted bacteria.20 Professional advice must be given as to the administration, caution, and type of oral product to be used.1 As of now, only chlorhexidine mouthrinses are administered clinically to patients with a prescription. For the most part, the public has turned to commercially available, over-the-counter mouthwashes that have deodorant-type properties to mask oral malodor instead of having antiseptic purposes. If a mouthwash’s antibacterial function comes from alcohol, which also enhances the flavor of the mouthwash, a slight dry-mouth effect may occur.1
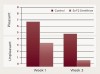
Triclosan is an antibacterial agent commonly found in many anti-acne products, hand soaps, and detergents. For many years, triclosan has been included in the toothpaste formulations to enhance inhibitory effects on bacterial metabolism in dental plaque. Numerous studies have confirmed these effects by showing a reduction in the accumulation of dental plaque, gingivitis, and calculus. One study revealed brushing twice a day with a triclosan toothpaste with or without tongue scraping significantly reduced the amount of bad breath caused bacteria.22 The triclosan-containing toothpaste was compared against the control, a standard sodium fluoride toothpaste. Using a Halimeter® (Interscan, www.halimeter.com) to measure the VSC concentrations, a reduction by more than 20 ppb was observed when measurements were taken at 3, 24, and 27 hours for 2 days.22 After using the triclosan toothpaste, participants reported in a questionnaire that their mouths overall felt “fresh and clean.” This demonstrates a simple regimen coupled with a triclosan-containing product can have profound effects against bad breath. Conversely, triclosan, essential oils, and cetylpyridinium chloride are still less effective in comparison to chlorhexidine for short-term management of oral malodor.23 The effectiveness of active ingredients in oral healthcare products depends on their concentration, in which excessively high concentrations can leave unpleasant side effects. Triclosan is not as potent as many other dentrifice compounds but nonetheless has anti-gingivitis and anti-plaque properties when used with other products that may contain stannous fluoride, chlorhexidine, essential oils, cetylpyridinium chloride, etc.24 Clinical studies have suggested the continued use of dentifrices and mouthwashes containing triclosan because these products amplify the effects of mechanical brushing and flossing to combat bad breath caused by bacteria.2 Other recent studies have shown the effectiveness of stannous fluoride in toothpastes for combating oral malodor.26 As a chemotherapeutic agent, stannous fluoride has wide-spectrum antimicrobial properties against both gram-positive and gram-negative species. Numerous clinical trials have demonstrated how well stannous fluoride acts against caries, plaque, gingivitis, and bad breath. These benefits are because of the multifaceted mechanisms of the stannous ion, from the alteration of bacterial growth to the inhibition of bacterial adhesion with the tooth surface to the inhibition of bacterial carbohydrate metabolism and enzymatic catalysis. Recently, a study attempted to evaluate the effect of 3 weeks’ use of a 0.454% stannous fluoride dentifrice on oral malodor, comparing it with a traditional 0.243% sodium fluoride dentifrice (the control). One of the two products was assigned randomly and blindly distributed to each of the 71 patients. Patients were asked to brush with their assigned products for 60 seconds twice a day for 3 weeks, and oral malodor was assessed on a 9-point hedonic scale26 as seen in Figure 1. The stannous fluoride dentifrice provided significantly lower mean hedonic scores than the control dentifrice at both Week 1 and Week 3,20 shown in Figure 2. These results suggested stannous fluoride provided a sustained significant improvement in oral malodor relative to a control dentifrice.26
If the oral malodor is caused by periodontitis, traditional scaling and root planing in the dental office may alleviate the depth of the periodontal pockets and severity of gingival inflammation.2 As a result, plaque elimination correlates with fewer odor-causing bacteria of the mouth. Treating malodor caused by periodontitis requires a careful initial evaluation and diagnostic plan,2 such as the one shown in Figure 3. Chlorhexidine can be administered to ease gingivitis and plaque buildup in patients with gingival disease.1 However, extended use of the product should be avoided because the rinse can discolor the teeth and tongue eventually. Overusing the product could cause resistance of certain bacteria to the formula and, therefore, lower its efficacy.1 Rather than for the main intention of treating oral malodor, chlorhexidine primarily is prescribed to cleanse underneath the gingiva of patients who have periodontitis. In turn, the rinse also relieves the mouth of foul odor after expulsing the accumulated bacteria. Patients may be advised to use oral irrigation systems with a chlorine dioxide mouthrinse to reach between teeth and under the gingiva; subgingival irrigation tips can be used if the pockets are deeper than 4 mm to 4.5 mm.27 An antimicrobial gel can be used to brush the gingiva, cheeks, and roof of the mouth, which should be left on without rinsing.27 Just as with all patients, providing oral hygiene education is a necessity for successful treatment of periodontal disease.2
Aside from the hygiene aspect, patients also can chew fibrous vegetables and sugarless gum to increase saliva flow and, in turn, help decrease oral malodor.1 Saliva functions as a buffering and cleaning agent that keeps bacteria at a manageable level in the mouth.1 Lastly, patients with oral malodor are encouraged to reduce or stop smoking, avoid offending foods, and eat at irregular intervals.27
Conclusion
Assessing oral malodor vigilantly from the beginning will enable dental professionals to treat each case appropriately. Sometimes the origins of the odors may stem from systemic diseases or side effects of certain drugs, and so these instances cannot be treated superficially. Then, the patient must be referred to a physician for further treatment based on the underlying causes.17 Other times, a patient who may not have true oral malodor insists he or she has it. Such patients with halitophobia should be referred to a psychologist for treatment. Through increasing investigation of this common concern, clinicians will one day be able to perform noninvasive procedures for diagnosing diseases by assessing differing odors, while more innovative products can help patients with oral malodor live comfortably and with self-confidence.17
About the Author
Sushma Nachnani, MS, PhD
Director, University Health Resources Group
Culver City, California
References
1. Nachnani S. The effects of oral rinses on halitosis. J Calif Dent Assoc. 1997;25(2)145-150.
2. Klokkevold PR. Oral malodor: a periodontal perspective. J Calif Dent Assoc. 1997;25(2):153-159.
3. Guggenheimer J, Moore P. Xerostomia: etiology, recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
4. Reisfield GM, Rosielle DA, Wilson GR. Xerostomia. 2nd ed. Fast Facts and Concepts. December 2008; 182.
5. Cochran S. Serax (oxazepam) causes xerostomia/dry mouth/cotton mouth. Associated Content. December 2008.
6. Hu Y, Hu DY, Zheng LL, et al. Establishment of malodor model and its effects on identifying the halitosis-related bacteria. Hua Xi Kou Qiang Yi Xue Za Zhi. 2007;25(3):226-229.
7. Krespi YP, Shrime MG, Kacker A. The relationship between oral malodor and volatile sulfur compound-producing bacteria. Otolaryngol Head Neck Surg. 2006;135(5):671-676.
8. Sterer N, Rosenberg M. Streptococcus salivarius promotes mucin putrefaction and malodor production by Porphyromonas gingivalis. J Dent Res. 2006;85(10):910-914.
9. Tyrrell KL, Citron DM, Warren YA, et al. Anaerobic bacteria cultured from the tongue dorsum of subjects with oral malodor. Anaerobe. 2003;9(5):243-246.
10. Quirynen M, Avontroodt P, Soers C, et al. Impact of tongue cleansers on microbial load and taste. J Clin Periodontol. 2004;31(7):506-510.
11. Hinode D, Fukui M, Yokoyama N, et al. Relationship between tongue coating and secretory-immunoglobulin A level in saliva obtained from patients complaining of oral malodor. J Clin Periodontol. 2003;30(12):1017-1023.
12. Hess J, Greenman J, Duffield J. Modelling oral malodour from a tongue biofilm. Journal of Breath Research. 2008;2(1):1-6.
13. Phillips M, Cataneo RN, Greenberg J, et al. Pilot study of a breath test for volatile organic compounds associated with oral malodor: evidence for the role of oxidative stress. Oral Dis. 2005;11(suppl 1):32-34.
14. Nalçacı R, Sönmez I. Evaluation of oral malodor in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(3):384-388.
15. Nachnani S, Majerus G, Lenton P, et al. Effects of training on odor judges scoring intensity. Oral Dis. 2005;11(suppl 1):40-44.
16. Baharvand M, Maleki Z, Mohammadi S, et al. Assessment of oral malodor: a comparison of the organoleptic method with sulfide monitoring. J Contemp Dent Pract. 2008;(9)5:76-83.
17. ADA Council on Scientific Affairs. Oral malodor. J Am Dent Assoc. 2003;134(2):209-214.
18. Tsai CC, Chou HH, Wu TL, et al. The levels of volatile sulfur compounds in mouth air from patients with chronic periodontitis. J Periodontal Res. 2008;43(2):186-193.
19. Tanaka M, Anguri H, Nonaka A, et al. Clinical assessment of oral malodor by the electronic nose system. J Dent Res. 2004;83(4):317-321.
20. Hughes FJ, McNab R. Oral malodour—a review. Arch Oral Biol. 2008;53(suppl 1):S1-S7.
21. Bordas A, McNab R, Staples AM, et al. Impact of different tongue cleaning methods on the bacterial load of the tongue dorsum. Arch Oral Biol. 2008;53(suppl 1):S13-S18.
22. Farrell, S, Baker, RA, Somogyi-Mann, M, et al. Oral malodor reduction by a combination of chemotherapeutical and mechanical treatments. Clinical Oral Investigations 2006;10(2):157-63.
23. van den Broek AM, Feenstra L, de Baat C. A review of the current literature on management of halitosis. Oral Dis. 2008;14(1):30-39.
24. Gunsolley, JC. A meta-analysis of six-month studies of antiplaque and antigingivitis agents. J Am Dent Assoc. 2006;137(12):1649-1657.
25. Gilbert P, McBain A, Sreenivasan P. Common therapeutic approaches for the control of oral biofilms: microbiological safety and efficacy. Clin Microbiol Infect. 2007;13(suppl 4):17-24.
26. Nachnani S, La S, Lee S, et al. Oral malodor reduction with 3-week use of 0.454% SnF2 dentifrice. Paper presented at: 86th General Session and Exhibition of the International Association for Dental Research; July 2008; Toronto, Canada.
27. Nachnani S, Clark GT. Halitosis: a breath of fresh air. Clin Infect Dis. 1997;25(suppl 2):218-219.