You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Warfarin is commonly used for patients with a history of atrial fibrillation (AF) to prevent cerebrovascular complications. The current evidence-based recommendations do not support the discontinuance of warfarin before dental extractions.1,2 Furthermore, intravenous recombinant tissue plasminogen activator (rt-PA) is used for patients with acute ischemic stroke, and achieving hemostasis in patients with recent dental extractions undergoing thrombolysis can be challenging. This article will provide a review of stroke prevention with oral anticoagulation and the dental management of acute stroke patients undergoing thrombolysis with recent tooth extraction. A case report of a patient who received rt-PA for an ischemic stroke after discontinuing warfarin prior to a single tooth extraction will be presented.
STROKE PREVENTION IN ARTIAL FIBRILLATION
Stroke is the leading cause of disability and the third leading cause of death in the US.3 Stroke presents as an acute neurologic deficit caused by brain infarction, which is the result of vascular occlusion or hypoperfusion of brain tissue. AF results in improper atrial contractions and, therefore, a lack of complete atrial emptying. This leads to blood stasis in the left atrium and thrombus formation. The thrombus then can migrate into the left ventricle and, with left ventricular contraction, be propagated to the systemic circulation. Emboli that travel to the cerebral vessels can result in stroke.4 AF is a potent risk factor for stroke and becomes one of the most common causes of stroke in those older than 70 years of age.5
Warfarin is used to prevent emboli in patients with AF, and the dosage is titrated by measuring the international normalized ratio (INR). The INR is a laboratory measurement of the time in which clot formation occurs. In 2001 the American College of Cardiology, American Heart Association, and European Society of Cardiology (ESC) published guidelines for the treatment of AF. Warfarin is recommended for all patients who have nonvalvular AF and at least one of the following risk factors: age 75 or older, prior stroke, transient ischemic attack (TIA) or systemic embolism, hypertension, decreased left ventricular function, or diabetes mellitus. For patients with nonvalvular AF and using warfarin for anticoagulation, an INR 2.0 to 3.0 is the goal. Warfarin has other indications, and the INR goals for other conditions vary. For those 65 to 75 years of age with none of these risk factors, either aspirin (325 mg/day) or warfarin can be used. For people younger than 65 years without such risks, aspirin is recommended.6
Warfarin acts as a vitamin K antagonizer. Clotting factors II, VII, IX, and X must undergo a vitamin-K dependent modification to be active. Warfarin treatment blocks this modification, resulting in the production of inactive clotting factors and consequently, increased clotting time as measured by the INR. The Food and Drug Administration’s (FDA) approved uses for warfarin include AF, prophylaxis of myocardial reinfarction, prosthetic cardiac valve component embolism, prophylaxis of pulmonary embolism, treatment of thrombotic disorders, and prophylaxis of venous embolism and thromboembolism.7
ACUTE STROKE TREATMENT
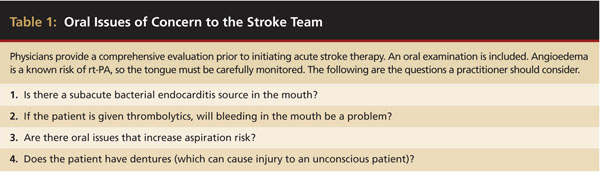
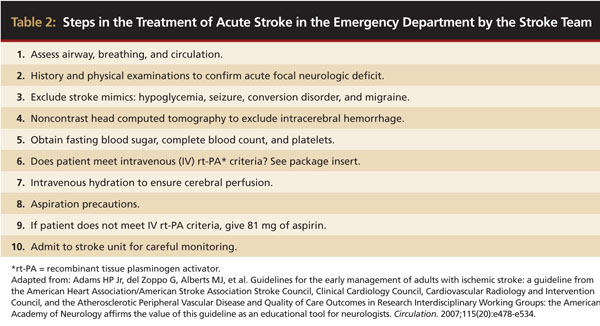
Current management for treatment of acute ischemic stroke includes the use of rt-PA within the first 3 hours after the stroke to disintegrate clots. This drug is administered intravenously and activates plasminogen in clots. Patients with stroke must meet specific criteria to qualify for rt-PA use and must have a computed tomography (CT) scan within the first 3 hours following symptoms to rule out a hemorrhagic stroke (Table 1 and Table 2). Table 1 is based on the authors’ clinical experience. Intravenous rt-PA is an effective therapy that is approved by the FDA for the treatment of acute ischemic stroke. However, because few patients arrive within the requisite 3 hours of symptom on-set, only 1% to 5% of patients who present with stroke receive this therapy.8 A literature search did not locate any articles discussing the effect of rt-PA on recent dental extraction sites.
 |
 |
In the two-part National Institute of Neurological Disorders and Stroke Recombinant Tissue Plasminogen Activator Stroke Study, the use of intravenous rt-PA was found to reduce permanent disability by an absolute margin of 11% to 14% and a relative margin of 30% to 50%, depending on the scale used.9 The use of rt-PA increases the risk of cerebral hemorrhage, the most dangerous complication of thrombolytic therapy.
Intravenous rt-PA must be commenced within 3 hours of witnessed symptom onset or the last time the patient’s condition was asymptomatic. The drug is much more beneficial the earlier it is administered, making stroke the quintessential medical emergency. A contraindication to rt-PA use is bleeding at a noncompressible site. No other thrombolytic is approved for the treatment of acute ischemic stroke.8
DENTAL EXTRACTIONS
Wahl reviewed reported cases of withdrawal from continuous oral anticoagulation for dental procedures. He found in 493 patients who underwent a total of 542 cessations of continuous oral anticoagulation, five cases (1.0% of patients; 0.9% of cases) had serious embolic complications with four deaths.10 Multiple studies have shown patients taking continuous oral anticoagulation can have limited extractions without postoperative hemorrhage when good surgical technique and local hemostatic measures are used.11-13 There have been zero studies involving extractions of more than five teeth per patient, removal of impacted teeth, or alveolar surgery.14 The research supports the current recommendations to not change anticoagulation for most extractions performed in a dental office.
The current evidence-based recommendations for treating patients receiving warfarin therapy were explained and supported with a literature review by Friedlander et al.2 For patients receiving warfarin with an INR between 2 and 3 requiring one to three simple dental extractions, the following recommendations apply: 1) consult with the physician to ensure that blood pressure is well controlled and the patient is not receiving additional antiplatelet therapy (aspirin and/or clopidogrel); and 2) inform the physician that local hemostatic measures can be used to control hemostasis and there is no dental indication to change to the warfarin regimen. For complex exodontia that includes removal of retained roots and impacted teeth, the dentist should limit the number of teeth to be extracted at one time, section teeth to limit ostectomies, remove all granulation tissue, place resorbable gelatin or oxidized cellulose material in socket, compress the wound, and place multiple interrupted sutures.2
Unnecessary postoperative antibiotics should be avoided because they can affect the digestive tract flora, and, in turn, impact vitamin K absorption and increase INR. The antibiotics that have been implicated include sulfamethoxazole/trimethoprim, amoxicillin, and amoxicillin plus clavulanic acid.15 Penicillin, which remains the first line of defense for infections in the oral cavity, was not found to be associated with overanticoagulation. Dentists should avoid nonsteroidal anti-inflammatory drugs (NSAIDs) for postoperative pain control because their effect on platelet function can lead to increased hemorrhage.16 Acetaminophen can be an effective analgesic for patients taking warfarin; however, it should be used with caution and for the shortest time possible because it can affect anticoagulation. Hylek et al found patients who took warfarin and consumed the equivalent of four regular strength tablets (325 mg) of acetaminophen for 7 days or longer increased their odds of having an INR greater than 6.17 The patient’s physician can be consulted if any postoperative medications that increase anticoagulation are required; additional INR testing may be needed.
Case Report
An 88-year-old male presented to the University of Michigan emergency department with difficulty speaking. His wife reported he had awakened with normal neurologic function and ate breakfast with her. At 7:30 am, he could not speak and his wife called 911. On arrival, the acute stroke team was activated, and examination revealed a severe global aphasia and mild right facial droop. He had no motor weakness, but he shook his right arm as if it did not feel normal to him and he could not communicate. Past medical history was significant for AF, pacemaker implantation, and hypertension, and his medications included digoxin, lisinopril, hydrochlorothiazide, and warfarin. Two days earlier in a dental office, the patient had undergone extraction of tooth No. 20. The wife reported he had been advised to discontinue the use of warfarin 5 days prior to the extraction. The warfarin had been restarted 36 hours previously to symptom onset, and he had taken two doses. It is unknown what the patient’s pre-extraction INR was when last checked. His INR in the emergency department was 1.3; however, platelets and other laboratory studies were normal. A head CT without contrast showed old periventricular white matter disease and no evidence of a cerebral hemorrhage or recent cerebral ischemia. On examination, the extraction site had light oozing.
The patient was considered for intravenous rt-PA because he was within the 3-hour window of symptom onset. Administration of rt-PA was planned. It was anticipated the extraction site would bleed significantly after administration, so the hospital dentistry service was consulted. It was believed any bleeding that would occur at the extraction site could be controlled with local measures. Following rt-PA administration, significant bleeding from the site was noted. Initially, the use of a folded gauze with biting pressure was attempted; however, it was not possible to achieve good biting pressure because of the patient’s fatigue and transient cognitive changes.
An alginate impression was taken bedside. The impression was poured in dental stone, and the cast was trimmed in the hospital dental laboratory. A 0.060-inch vacuum formed splint was fabricated (Figure 1). Cellulose dressing (Surgicel®, ETHICON, Inc., www.ethicon.com) was folded into a square and placed directly on the socket. The vacuum-formed splint was placed over the extraction site to apply pressure and to secure desired position (Figure 2). Hemostasis was achieved, and the splint was kept in place for 2 days. On removal, bleeding ceased, and the patient was subsequently discharged.
DISCUSSION
The exact cause of this patient’s acute stroke is unknown. The patient had a significant medical history of AF and anticoagulation therapy for stroke prevention. However, on presentation to the hospital, his INR was not within the therapeutic range after discontinuation of oral anticoagulation for 5 days. It is possible but not certain that his stroke would have been prevented if warfarin was not discontinued. In this case, acute stroke was successfully treated using rt-PA. Following rt-PA therapy, the hospital dentistry team was able to manage the extraction site using local measures to prevent hemorrhage.
CONCLUSION
This case report illustrates the importance of careful control of INR during dental treatment. The dentist and physician need to communicate to ensure patients are not receiving too much anticoagulation therapy. In most cases, patients who receive anticoagulation treatment for stroke prevention and have an INR within therapeutic range should not discontinue oral anticoagulation before tooth extraction. If a dentist does not feel comfortable performing extractions in a patient receiving anticoagulation treatment, he or she should make a referral to an oral surgeon or a hospital-based dentist rather than interrupting the patient’s anticoagulation regimen. Dentists should be conscious of the ways in which the medications they commonly prescribe can affect a patient’s anticoagulation status.
Dentists are likely to play an important role for patients who recently received thrombolytics and exhibited oral bleeding. Ability to provide measures for hemostasis at recent extraction sites is an important part of the acute stroke intervention.
REFERENCES
1. Jeske AH, Suchko GD; for ADA Council on Scientific Affairs and Division of Science; Journal of the American Dental Association. Lack of a scientific basis for routine discontinuation of oral anticoagulation therapy before dental treatment. J Am Dent Assoc. 2003;134(11):1492-1497.
2. Friedlander AH, Yoshikawa TT, Chang DS, et al. Atrial fibrillation: pathogenesis, medical-surgical management and dental implications. J Am Dent Assoc. 2009;140(2):167-177.
3. Miniño AM, Heron MP, Murphy SL, et al; Centers for Disease Control and Prevention National Center for Health Statistics National Vital Statistics System. Deaths: final data for 2004. Natl Vital Stat Rep. 2007;55(19):1-119.
4. Fishman MC, Hoffman AR, Klausner R, et al. Medicine. 5th ed. In: Marquardt N, ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.
5. Rodgers H, Greenaway J, Davies T, et al. Risk factors for first-ever stroke in older people in the north East of England: a population-based study. Stroke. 2004:35(1):7-11.
6. Fuster V, Rydén LE, Asinger RW, et al; American College of Cardiology/American Heart Association/European Society of Cardiology Board. ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences (Committee to Develop Guidelines for the Management of Patients with Atrial Fibrillation): developed in collaboration with the North American Society of Pacing and Electrophysiology. J Am Coll Cardiol. 2001;38(4):1231-1266.
7. Hirsh J, Fuster V, Ansell J, et al; American Heart Association/American College of Cardiology Foundation. American Heart Association/American College of Cardiology Foundation guide to warfarin therapy. J Am Coll Cardiol. 2003;41(9):1633-1652.
8. Albers GW, Amarenco P, Easton JD, et al. Antithrombotic and thrombolytic therapy for ischemic stroke: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 suppl):483S-512S.
9. Kwiatkowski TG, Libman RB, Frankel M, et al; the National Institute of Neurological Disorders and Stroke Recombinant Tissue Plasminogen Activator Stroke Study Group. Effects of tissue plasminogen activator for acute ischemic stroke at one year. N Engl J Med. 1999;340(23): 1781-1787.
10. Wahl, MJ. Dental surgery in anticoagulated patients. Arch Intern Med. 1998;158(15):1610-1616.
11. Blinder D, Manor Y, Martinowitz U, et al. Dental extractions in patients maintained on oral anticoagulant therapy: comparison of INR value with occurrence of postoperative bleeding. Int J Oral Maxillofac Surg. 2001;30(6):518-521.
12. Devani P, Lavery KM, Howell CJ. Dental extractions in patients on warfarin: is alteration of anticoagulant regime necessary? Br J Oral Maxillofac Surg. 1998;36(2):107-111.
13. Morimoto Y, Niwa H, Minematsu K. Hemostatic management of tooth extractions in patients on oral antithrombotic therapy. J Oral Maxillofac Surg. 2008;66(1):51-57.
14. Ward BB, Smith MH. Dentoalveolar procedures for the anticoagulated patient: literature recommendations versus current practice. J Oral Maxillofac Surg. 2007;65:1454-1460.
15. Vissir LE, Penning-van Bees FJ, Kasbergen AA, et al. Overanticoagulation associated with combined use of antibacterial drugs and acenocoumarol or phenprocoumon anticoagulants. Thromb Haemost. 2002;88(5):705-710.
16. Kniff-Dutmer EAJ, Schut GA, van de Laar MA. Concomitant Coumarin-NSAID therapy and risk for bleeding. Ann Pharmacother. 2003;37(1):12-16.
17. Hylek EM, Heiman H, Skates S, et al. Acetaminophen and other risk factors for excessive warfarin anticoagulation. JAMA. 1998;279(9):657-662.
ABOUT THE AUTHORS
Aimee Picard, DDS
General Dentist, Erie Family Health Center, Chicago, Illinois
Samuel Zwetchkenbaum, DDS, MPH
Section Chief, Hospital Dentistry, Department of Oral and Maxillofacial Surgery/Hospital Dentistry, University of Michigan School of Dentistry, Ann Arbor, Michigan
Lewis B. Morgenstern, MD
Professor and Director of the Stroke Program, Department of Neurology, University of Michigan Medical School,
Ann Arbor, Michigan

